Disclaimer: Content for entertainment purposes only. Not medical or health advice.
A few weeks back a friend messaged me asking if I’d written anything explaining why sugar is not bad.
While she has left her years of sugar demonization behind (and is feeling better than ever), she has been feeling frustrated with those around her who are still convinced that sugar is “the white death” and proceed to either attempt to lecture her or give her the side eye for eating it.
Her message made me realize that I’ve yet to write something that addresses all the sugar confusion and myths in one place. While many of my articles dive deep into debunking myths such as “sugar causes glycation and ages you,” “cutting out sugar cures cancer,” or “sugar causes diabetes,” I’ve yet to create something that would summarize all of these points and debunk all the myths in one place. This article is that place.
For anyone who might be new here, let me address a few points right off the bat.
No, I am not sponsored by the sugar industry. In fact, my only “sponsors” are those who find my writing interesting enough to become paid subscribers here on Substack. (Thank you for making it possible for me to feed myself and keep a roof over my head ❤️).
No, I do not want people to become obese, diabetic, or cancerous. Quite the opposite, actually. Global sugar consumption is decreasing, more and more foods and beverages are substituting sugar with sugar-free sweeteners due to sugar taxes, “going sugar-free” has become synonymous with “health,” and every tabloid, talk show, and even your uncle Jerry with his latest foray into the world of keto are convinced that sugar is poison. Even in the United States, sugar consumption has been on a decline since the 1990s.1 Yet, obesity, diabetes and cancers are still on the rise more than ever. Perhaps the cause behind these diseases is far more multifaceted, and “sugar bad” is far too simplistic of an explanation, implicating sugar without it being a causative factor at all?
No, I do not want people to consume the Standard American Diet nor do I think that nutrient-void ultra-processed foods should be part of anyone’s dietary regimen. There’s a peculiar phenomenon where whenever the word “sugar” is mentioned, it’s assumed that the “sugar” in question means donuts, cupcakes, candies, or a bottle of Mountain Dew. Do these foods contain sugar? Yes. (Although, in the United States at least, this sugar rarely comes in the form of white table sugar and instead comes in the form of corn syrup). However, these foods also often contain 20+ other ingredients, many of which aren’t even food, for example, titanium dioxide, carrageenan (a carcinogenic gum that’s not only damaging to the gut but also can trigger a severe latex allergy), excitotoxic food colourants (such as red-40), or hexane-extracted canola oil. Calling a donut “sugar” just because it contains sugar would be like calling a hamburger “onion.” These other ingredients, plus the fact that these Franken-foods are almost entirely micronutrient-void, hypercaloric and are also often heavily contaminated with toxic metals and petroleum byproducts during production2 are what makes them awful, as opposed to their sugar content. If someone’s diet consists mainly of pre-packaged, micronutrient-void, long-shelf life abominations that unfortunately carry the label “food,” they will obviously feel awful. Again though, it’s not the sugar.
Part of the reason why I’m writing this is because this “sugar bad” sentiment leads people to poor dietary choices.
On the one hand, if you believe that it’s the sugar that makes processed “junk food” bad, this logic will lead you to believe that this processed “junk food” is no longer bad once sugar is removed from it and replaced with a sugar-free sweetener. By this logic, you might decide that sugar-free junk food variants are fine to put back on the menu. However, removing sugar from crappy foods doesn’t turn them into gold. They are still crappy foods. Except now probably the one good thing about them (the substrate for cellular energy generation, aka sugar) has been removed. Sugar-free variants of junk food are not healthy dietary choices, especially since artificial sweeteners don’t come without their risks (although that’s a topic for another article).
On the other hand, if someone realizes that, biochemically, all carbohydrates are sugars (whether white table sugar, potatoes or apples), and if they believe that it’s the sugar that makes these foods “evil,” they might arrive at the conclusion that all sources of sugar need to be cut out, and to be healthy, they must follow a ketogenic or carnivore zero-carb diet. This, however, is not the solution.
The ketogenic diet leads to nutrient and mineral imbalances due to altered nutrient retention, and lowers the levels of the active thyroid hormone, leading to downstream decreases in sex hormones such as testosterone and progesterone. These hormones are needed, among other things, for fertility and healthy aging. The issues with ketogenic diets are covered in detail in my article on the carnivore diet. Since the body can convert protein and fat into sugar, and since the stress hormones that become elevated due to carbohydrate avoidance and the consequent lowering of thyroid hormones elevate the rate of sugar synthesis in the body while impairing its burning for energy, those who go keto often paradoxically find themselves with higher-than-before blood glucose levels. I talk about this in my article on diabetes. Ketones are also stronger glycating agents than sugar. I talk about this in my article on glycation.
Another part of the reason why I am writing this is because I too once believed that sugar is the cause of all evil. I read countless publications which claimed sugar to be inflammatory, metabolically damaging, and the root of our current obesity, cancer and diabetes epidemic. I spent years eating a low-carb paleo diet, which only led me to new health problems. Since the only advice I seemed to come across back then was that all my issues were likely due to sugar, I decided to cut back even more: pursuing a keto-carnivore diet. Not only did that not solve my issues, but it actually resulted in my thyroid, gut and sleep issues getting worse over time, paired together with fat gain and higher fasting blood sugar. Just like many others, I too suffered from cognitive dissonance which somehow prevented me from noticing that whenever I “cheated” on my “healthy” diet and ate something containing sugar in its simplest forms, my headaches would subside, my sleep would improve, and my menstrual cycle would become more regular. After crashing and burning following my keto experiment, I had to really question my beliefs and further investigate my long-held nutrition assumptions.
Now, after having apologized to sugar and introduced it back into my diet (in the form of fruit, juice, potatoes, bread, honey, maple syrup, desserts made with real, whole food ingredients, and yes, also white table sugar), my digestion is better than ever, my menstrual cycle is asymptomatic, I can eat more than ever without putting on fat, I don’t get sick as often, and my mental and physical wellbeing is overall a lot more stable.
Lastly, yet another part of the reason why I’m writing this is that I am simply annoyed with inaccurate information and the epidemic of cognitive dissonance that many registered dietitians and nutrition authorities seem to suffer from.
Many of them will preach that white table sugar (which is entirely micronutrient void and gets broken down into free glucose and fructose molecules in the gut before absorption) is a poison, yet white rice (which is also entirely micronutrient void and gets broken down into free glucose molecules in the gut before absorption) is a “healthy source of dietary carbohydrates.” The one difference between the two is that, unlike white rice, table sugar contains fructose. However, if the logic is that it’s the fructose that makes table sugar a poison then why is it that…fructose is the main sugar in fruits and vegetables, the foods that these same nutrition authorities tell us are the healthiest foods we can eat? If you’re reading this and thinking that this logic makes no sense, then I say “Great.” Now we are on the same page.
Since I want this article to be the place that addresses all the sugar myths and misconceptions, here’s a summary of topics covered in this article:
In this article:
Most People Have No Idea What Sugar Is
Why Do Some People Feel Better After Going “Sugar-Free?”
The Case for Sugar Being Good for Us
Sugar Increases Your Metabolism
Sugar Is Pro-Fertility
Sugar Protects Against Stress
Sugar Protects Against Leaky Gut
Sugar Promotes Wound Healing
Sugar Is Liver Protective
Sugar Makes You Smarter
Sugar Supports Healthy Immune Function
What About Research Showing the Adverse Effects of Dietary Sugar?
Is Added Sugar “Bad,” But Natural Sugar “Good”?
Hypercaloric, High Fat, High Sugar, Highly Processed Diets are Not “High Sugar Diets”
Rodents Have a Lower Sugar Tolerance Than Humans
Busting Sugar Myths and Misconceptions
Sugar Isn’t the Cause of High Blood Glucose Levels
Sugar Isn’t the Cause of Insulin Resistance
Sugar Doesn’t Damage Your Metabolism or Cause Inflammation
Sugar Doesn’t Cause Cancer or Diabetes
Sugar Doesn’t Cause Glycation and High HbA1C
Sugar Isn’t “Empty Calories”
Sugar Isn’t Something that Only Young, Lean People Can Eat
Sugar Isn’t Addictive
Sugar Doesn’t Cause Cavities
We Are Vilifying Sugar Instead of Focusing on the Real Problems
To make sure that we are all on the same page, let’s start by first discussing something that really bothers me. Namely that…
Most People Have No Idea What Sugar Is
To begin this article, let’s start with answering a question that can get us all on the same page. The question is: “What is sugar?”
I realize that many people might think that this question is silly. However, what is interesting about the widespread fear of sugar is that many people don’t really understand what sugar is.
Usually, the word “sugar” is associated with the white stuff that comes in a bag and is derived from either sugar beets or sugar cane.
White table sugar is composed entirely of sucrose. Each sucrose molecule consists of glucose and fructose molecules held together by a glycosidic bond (think of them as glucose and fructose holding hands).
Do you know what else contains sucrose?
Fruits, such as apples, apricots, bananas, cherries, figs, grapefruits, grapes, kiwis, mangoes, nectarines, oranges, papayas, peaches, pears, pineapples, plums
Vegetables, such as peas, sweet potatoes, beets, carrots, turnips, onions
Culinary fruits, such as bell peppers, eggplants, pumpkins, squashes, zucchinis, tomatoes
Various grains, legumes and some nuts in smaller amounts
Many people aren’t aware of this. It isn’t rare to see someone declare that they will be starting a “sugar-free” diet of mostly fruits and vegetables, not realizing that sucrose (the very same thing as white table sugar) is also found in these foods.
Knowing that sucrose is found in real, whole foods, kind of puts a stake in the idea that sugar is akin to a poison and that putting some in your morning coffee is akin to “literally snorting cocaine.”
Honey, agave syrup and corn syrup are also made up of fructose and glucose. However, in these foods, most of the fructose and glucose are not held together by glycosidic bonds. Instead, they exist as free fructose and free glucose, as opposed to sucrose. Free glucose and free fructose are also found in varying amounts in fruits, vegetables, culinary fruits, and other plant foods.
Starches (savoury carbohydrate sources, such as potatoes, rice, or wheat flour) consist of chains of multiple glucose units held together by glycosidic bonds. When you chew starches long enough, they start tasting sweet. This is because amylase, an enzyme produced by your saliva, starts breaking down the bonds and releasing free glucose for absorption by your gut.
Milk (and other non-fermented dairy products) contain lactose, which, after being broken down by the enzyme lactase in the small intestine, separates into molecules of glucose and galactose before absorption.
Additionally, meat, mushrooms, fish and eggs contain the sugar ribose. Ribose can be converted into glucose in the body in the process of gluconeogenesis.
In short, fruits, vegetables, grains, tubers, meat and dairy all contain sugars.
Now that we have established that basically most whole foods contain sugars (whether in the form of sucrose or another form), let’s address another way in which the “sugar bad” argument gets spun, namely the naturalistic fallacy that “real sugar in food is good, but added sugar is bad.”
With a basic understanding of food biochemistry, it becomes apparent that all carbohydrates are sugars and that protein foods can turn into sugars in the body during stressful conditions. With that, the “sugar is the cause of all evil” argument starts to lose its footing since it would become akin to saying “food is evil.” This then morphs this argument into “added sugar is bad,” or sometimes into claiming that anything that tastes sweet is bad, such as:
“When you add sugar (sucrose) to a pre-packaged food then it’s bad, but if a food naturally has sucrose, then it’s good.”
“When a pre-packaged food tastes sweet (because it contains glucose and fructose) then it’s bad. When a pre-packaged food doesn’t taste sweet (because it contains only glucose as starch, which is still sugar) then it’s good. When a fruit tastes sweet (because it contains glucose and fructose) then it’s good.”
Many of the people who “quit sugar,” such as the man in the viral video below, do precisely that: they cut out pre-packaged food that tastes sweet and has added sugar, and claim that they “quit sugar,” while still eating rice, potatoes, pasta and fruit (or, in other words, sugar).
To start, this is not a stab at the man in the video. I am happy that he wanted to take the initiative to improve his health and his dietary habits. Sadly, he is just as misguided as I was in the past.
If you watch the video, at the start he makes some well-intentioned yet misguided claims regarding why “sugar is bad,” and then proceeds to show how his diet changes after quitting sugar. In short, he stops snacking on granola bars and breakfast cereal all day and replaces them with relatively balanced meals of white rice, greens and lean meat. He feels better, loses weight, and attributes this to quitting sugar (which he hasn’t quit). A more appropriate title for this video would be: “I quit eating like an unsupervised toddler snacking on nutrient-void convenience store food all day and started eating home-cooked meals like a grown adult for 30 days, and now I *gasp* feel better.” It doesn’t make for a great video title but is a far more accurate description.
Again, I want to make clear that I have nothing against the man in the video and the saltiness of the above paragraph is simply a reflection of my annoyance at how misunderstood the word “sugar” is. While this annoyance might seem like a mere annoyance at semantics at this point in the article, the rest of this article will make it clear that failing to be as nit-picky about the issue as I am being here snowballs into some pretty serious consequences concerning nutritional policy and colloquial understanding of the effects of carbohydrates on physiology.
Now that we are on the same page as to our understanding of “what is sugar,” let’s start exploring the topics listed near the top of this article. As a reminder, some of these specific topics have already been addressed in more of a “deep dive” manner in my other articles. While this article will summarize the key points, if you want to read more on these topics, together with plenty more references and studies cited, I invite you to check out the other articles which I’ll be mentioning throughout.
Why Do Some People Feel Better After Going “Sugar-Free”
Since many of you might be asking “If sugar is good, then why do so many feel better after going sugar-free?” let’s dive into it.
Whether a person decides to go “pseudo-sugar-free” (by simply cutting out cookies, candies and sweet convenience foods with added sugar), or by going truly sugar-free (keto), both of these dietary changes tend to have a few things in common:
Generally when a person decides to “cut out sugar,” they do so after consciously deciding to improve their dietary and lifestyle choices. As in the case of the man in the viral video linked above, many others who decide to go “sugar-free” similarly make more fundamental changes to their nutrition, including eating more real, whole foods, fewer pre-packaged long shelf-life foods, and more home-cooked, satiating meals. This results in a diet that is generally more nutrient-dense. Micronutrients (vitamins and minerals) enable our cells to burn macronutrients (carbs, fats and, if necessary, protein) for energy. When these micronutrients are in short supply, our cells have a hard time burning fuel for energy. The body is then more likely to deposit the potential fuel from food as body fat instead of extracting energy from it, even if our energy needs haven’t been met yet, leaving us feeling fatigued and symptomatic. In short, when most people decide to do a “low carb diet,” they inadvertently end up doing a “low crap diet.”
Taking the initiative to improve one’s diet often comes with the initiative to make other lifestyle improvements, such as working out, spending more time outside, and avoiding alcohol. All of these will make a person feel better.
Many conventional “snack foods” that might be available in work break rooms or that a person might keep in their cupboard are sweet-tasting foods that the average person is likely to label as “sugar.” When a person chooses to stop eating those foods, they often unconsciously stop snacking altogether (similar to the man in the video). This results in the person unconsciously entering a caloric deficit. This will often lead to fat loss (at least temporarily, until metabolic adaptation takes place). Since excess body fat is inflammatory (it releases inflammatory cytokines and can make it harder for the body to burn sugar for energy, more on this in a bit), becoming leaner will likely make a person feel better. Still, the sugar wasn’t the problem. The problem was the person’s habit of snacking on high-calorie, nutrient-void foods which likely exceeded their body’s daily caloric needs and resulted in fat gain.
When someone decides to pursue a carnivore or ketogenic diet, other additional factors can improve their well-being and general health, at least short term.
First, many people might suffer from mild allergies or intolerances to certain foods, including foods which are conventionally perceived as healthy, such as whole grains or vegetables, in part due to gut dysbiosis or bacterial overgrowths. A carnivore or keto diet is often the ultimate elimination diet that gets rid of foods that might cause inflammation for some, or that might feed pathogenic bacteria, which produce inflammatory mediators (such as endotoxin and histamine). However, eliminating foods forever isn’t the solution. Addressing thyroid health, dysbiosis and gut health are the real solutions. I go deeper into this in my article on the carnivore diet and my article “How to Finally Heal Your Gut,” where I explain how thyroid health controls gut health.
Additionally, most chronic diseases (including diabetes type 2, Alzheimer’s disease, and even cancers) are characterized by impairments in the body’s ability to extract cellular energy from glucose. While glucose is our cells’ preferred fuel source, factors like vitamin and mineral deficiencies, bacterial endotoxin, low oxygen levels, high levels of fat in the blood, stress, and low levels of thyroid hormones, among other factors, can interfere with cells’ ability to efficiently and completely burn glucose for energy. However, these impairments are not caused by glucose (sugar) itself. Factors that contribute to impaired glucose metabolism will be discussed in more detail in later parts of this article.
On a zero-carb diet, cells are supplied with a greater supply of fats and ketones, providing them with alternative fuel sources that they can use to extract cellular energy if they struggle to extract energy from glucose well. While the brain is unable to fully switch to a fuel source other than glucose, some parts of the brain can use ketones as a fuel alternative in place of glucose. The availability of ketones can bring on improvements in certain disorders of the brain, as the brain is given an alternative way to produce cellular energy. The failure of cells (whether systematically or in a specific organ) to produce and use adequate cellular energy is at the root of most if not all disorders, something that I talk about in my other articles, including my articles on the bioenergetic view of health (Dr. Ray Peat’s work), diabetes, hypothyroidism and PCOS. Plus, when cells fail to fully oxidize glucose for energy, some of the byproducts of glucose metabolism can be detrimental and can increase oxidative stress. I talk about this in my series on glycation.
In short, a failure in cells’ ability to generate and use cellular energy is behind most if not all health issues. If cells are struggling with deriving energy from glucose (for example, due to vitamin and mineral cofactor deficiencies), giving them fat and ketones will provide alternative routes for generating energy and replenishing their energy stores. This is what’s behind the improvements in blood labs, fertility, mental symptoms and physical ailments that some see on low-carb/no-sugar diets.
However, even when eating zero carbs, the liver will always produce glucose and supply it to the bloodstream. Because of this, the temporary symptomatic improvements on low-carb diets are rarely long-lived, especially since they worsen the underlying dysfunction in glucose metabolism. High-fat diets further damage cells’ ability to burn glucose well, and the stress hormones that become elevated on low-carb diets cause the wasting of important minerals needed for glucose metabolism, such as magnesium. I provide sources backing up these statements in my article on diabetes.
What this means is that the symptomatic improvements seen on low-carb diets are not only often relatively short-lived but are also worsening the dysfunction “under the hood.” This is why so many famous keto/carnivore influencers (such as Thomas Delauer, Dr. Shawn Baker, or Dr. Paul Saladino, to name a few) eventually hit a wall with their health and start introducing carbohydrates again.
The long-term solution to metabolic illness isn’t to avoid glucose (it can’t be done), but to make our cells better at utilizing glucose for energy.
The Case for Sugar Being Good for Us
Before I get into busting sugar myths, let’s talk about something which is rarely discussed. Namely, how sugar can benefit our health.
We know that fruits, which are a major source of naturally occurring sucrose in our diets, are health-promoting foods. However, their healthful effects often get attributed to their vitamin, mineral and flavonoid content. For the sake of this article, to shatter some assumptions and shake up some preconceived notions, I will go over the health benefits of plain sucrose - aka pure white table sugar.
First, let me address why sugar would have health benefits.
If you’ve been a long-time reader of my Substack you know that I talk a lot about how the body’s health is downstream from the health of the smallest units making up our body: our cells. For our cells to remain healthy, they need to be able to create adequate cellular energy out of the foods that we eat. This cellular energy is then used by our cells to maintain themselves, power all of their functions, keep their structure, and repair defects. Whenever the cells that make up our tissues and organs lack energy, those organs and tissues will start lacking energy as a whole, manifesting in their malfunction. This shows up as various disease states. This larger view of health is discussed in my articles on the bioenergetic view of health (Dr. Ray Peat’s work) and hypothyroidism.
What does sugar have to do with this? Well, glucose is the preferred fuel source for most of our cells, one that provides the most units of energy (ATP) per molecule of oxygen, and one that results in the creation of fewer reactive oxygen species during the energy generation process compared to fat.3 In simpler terms, this means that cells can derive energy from glucose quicker than they can derive energy from fats, with a lesser risk of damage to their structure.
“More ATP is produced per O2 consumed when glucose is oxidized, compared with when fat is oxidized.”4
Fructose, which is the other component of sucrose (table sugar), has other unique benefits, including being the fuel of choice for our reproductive cells. For example, sperm cells use fructose for energy and if they run out of fructose, they can’t survive and fertilize the egg.5 Fructose is also the main sugar in amniotic fluid (the fluid in which a fetus grows during pregnancy), and in fetal blood, where not only is it used as a primary source of energy for growing the baby, but also acts as a signalling molecule used to guide proper growth and development.6
Fructose has also been shown to help the body get rid of alcohol quicker.78
“The administered dose of fructose significantly (P < 0.05) reduced the duration of alcohol intoxication by 30.7%, and accelerated the elimination (metabolism) of alcohol from bloodstream by 44.7% (P < 0.05).”9
That being said, let’s jump into the specific studies looking at the benefits of simple sucrose.
Sugar Increases Your Metabolism
Our metabolic rates are controlled by our levels of the active thyroid hormone, triiodothyronine (T3). When we have a shortage of this hormone, our metabolism slows down.
Adequate levels of T3 are needed for the proper function of every single cell in the body, as the rate at which our cells can create cellular energy out of the foods that we eat is controlled by this hormone. Low thyroid hormone levels, also known as hypothyroidism, show up in endless, multifaceted ways. The most common manifestations are cold hands and feet, low body temperature, hair loss, constipation, dry skin, and a propensity towards fat gain.
Sucrose has been shown to increase the conversion of the thyroid pro-hormone, thyroxine (T4), to the active thyroid hormone (T3), increasing thyroid hormone levels in the body. Artificial sweeteners had the opposite effect.1011 Sucrose increases active thyroid hormone levels by supporting the conversion of T4 to T3 by the liver.
Sucrose also helps to lower cortisol levels. Cortisol interferes with the conversion of T4 to T3 by the liver.12
Due to this effect, eating sucrose has been shown to increase the basal metabolic rate13 and increase body temperature.14 When participants were fed an excess of calories, with this excess coming from either fat or sugar, the sugar group saw a larger increase in their daily caloric expenditure.15 That is, they were able to get away with increasing their calories more without it resulting in weight gain.
In other words, sucrose, when eaten as part of a diet that isn’t excessively high in calories, can actually help with fat loss. Research has found that diets high in sugar and low in fat are negatively associated with obesity.16
Sugar Is Pro-Fertility
In women, progesterone is the main hormone involved in maintaining pregnancy. A drop in progesterone at the end of pregnancy is what triggers labour.
When preterm labour takes place, the baby born prematurely often suffers from lung, liver or other disorders, as their organ systems weren’t given enough time to properly develop.
At the end of pregnancy, cortisol levels (cortisol is our main stress hormone) rise. This rise in cortisol is considered to be one of the mechanisms behind labour onset. Since cortisol has an anti-progesterone action, if it rises too high, it can block progesterone.17 The drop in progesterone then leads to the start of the birthing process.
However, if this progesterone drop happens prematurely, a woman can either miscarry or experience pre-term labour.18 This is why stressful events are known to cause miscarriages. The lower a woman’s progesterone levels are, the lower the threshold at which cortisol can induce labour. The higher a woman’s cortisol levels are, the harder it becomes to maintain a pregnancy.
Sugar (sucrose) is known to lower cortisol levels (which is why the body tends to crave sweets when stressed). When pregnant rats were given sucrose, they had higher levels of progesterone in their blood and the brain, together with lower levels of the stress hormones cortisol and adrenaline.19
In one human experiment, where men’s sperm quality was being assessed, men were asked to follow a healthy diet, prepared for them by a dietician, for one week. Afterwards, they were given the same diet for another week, with the addition of 375 grams of extra sugar per day (that’s a lot!). What did the study find? Their sperm quality increased on the sugar-supplemented diet!20 Not only that but during the sugar-supplemented diet, they put on muscle mass. This study shows that the addition of sugar to an already healthy, micronutrient-rich diet can be beneficial by providing the body with an additional supply of its preferred energy source.
“The simultaneous increase of sperm motility and lean mass indicates that 1 week of a high-sugar diet on top of a healthy baseline had an anabolic effect in our young, healthy, and lean participants.”21
Sugar Protects Against Stress
Probably one of the most multifaceted ways in which sucrose can be beneficial is by dampening the stress response and protecting us against the negative effects of elevated stress hormone levels.
Glucocorticoids (such as cortisol) and catecholamines (such as adrenaline) are our built-in danger protection mechanism. When our bodies and/or minds sense danger, these hormones elevate to help us survive our fight against or flight from the danger at hand. Cortisol stimulates the liver to produce glucose (to ensure a steady fuel supply for the brain and nervous system in times of danger) and blocks insulin signalling. Adrenaline stimulates the release of fat from our fat stores into the blood, to provide extra fuel sources for other tissues. These mechanisms are meant to save us in times of acute stress. However, in today’s world, various psychological and physiological factors can cause these hormones to become chronically elevated. When chronically elevated, these hormones can contribute to physical symptoms like fat gain, muscle wasting, and insulin resistance (more on this later), together with psychological disturbances like anxiety, depression and hopelessness. These are only some of the risks.
Sucrose lowers cortisol in response to both current and past psychological and physiological stressors.
“Excessive, repeated or chronic activation of the HPA axis and SNS [sympathetic nervous system] has a number of negative consequences. For instance, excessive glucocorticoid exposure is associated with cognitive decline and diminished bone density, while persistent elevations in SNS drive are linked with cardiovascular dysfunction […] HPA axis activity can be profoundly inhibited by the metabolic properties of sucrose.”22
In one study in which a stress test required participants to put their hands in cold water, those who consumed more sugar had a lower cortisol response to the test,23 demonstrating that sugar consumption can make the body perceive stressors as less stressful.
Hopelessness is a learned belief that a stressor cannot be escaped so there is no point in trying to escape it in the future. Learned hopelessness usually develops as a consequence of chronic stress. In humans, learned hopelessness shows up as a belief that your situation is, well, hopeless and that you can’t do anything to better your life. It can manifest as passivity and decreased motivation. Sugar can help protect against learned hopelessness. In animal experiments, when rats were exposed to inescapable stress (which usually results in animals developing learned hopelessness), they didn’t develop hopelessness if they drank water with sucrose or glucose afterwards.2425
Sugar Protects Against Leaky Gut
In my digestion article, I already talked about how ketogenic diets have been shown to increase intestinal permeability. This is partially caused by how ketogenic diets affect the microbiome and partially because the cells that make up the intestinal wall have a much harder time making energy out of ketones than out of glucose. The lack of adequate fuel from carbohydrates on keto diets can affect these cells’ ability to make adequate cellular energy, contributing to a leaky gut.
However, plain ol’ sucrose itself has been shown to be protective of the gut. Probably anyone who has dipped a bit more than their toes into the health and nutrition world has heard of anti-nutrients. The label “anti-nutrients” refers to certain compounds, often present in significant amounts in improperly prepared plant foods, which can inhibit the absorption of certain micronutrients while also being damaging to the gut. Did you know that sucrose can protect against the deleterious effects of some anti-nutrients?
In one experiment,26 when rats were given either a diet containing lectins (a type of anti-nutrient) from improperly prepared beans, or a diet containing lectins and sucrose, those given sucrose had lower rates of leaky gut. Additionally, rats given a diet with lectins had a significant increase in bad gut bacteria translocating to the liver. Bacterial translocation to the liver can increase cholesterol levels and cause fatty liver disease. When sucrose was added to the lectin diet, it completely prevented bacterial translocation to the liver.
In short, sucrose protected them against lectin-induced leaky gut and endotoxin-induced liver problems that can arise as a consequence of leaky gut.


As mentioned earlier, sucrose lowers cortisol levels, and cortisol levels (which become elevated in times of chronic stress) are known to cause intestinal permeability, aka leaky gut. By supplying gut cells with energy, protecting against anti-nutrient induced damage and lowering cortisol, it seems that sucrose can protect the gut lining in multiple ways.
Sugar Promotes Wound Healing
Sugar, for centuries, has been used as a topical remedy to promote wound healing. By applying sugar to a wound, you can provide fuel for the damaged tissue cells and the immune cells present at the site of injury.
Sugar also promotes the creation of new blood vessels at the site of injury (which helps to bring nutrients and other supplies necessary for healing to the wound).27 When applied to wounds, sugar is also an extremely effective antibacterial agent, as it helps to remove moisture from the wound. This moisture could otherwise act as a bacterial breeding ground. The application of sugar to wounds fends off infections and stops wounds from developing a foul smell.
“Sugar has been used on wounds for more than two centuries. Pure sugar will produce a sterile environment at the wound surface because its water activity (ie the ratio of vapour pressure produced by sugar to the vapour pressure of pure water) is very low. In other words, the removal of water prevents bacteria from multiplying and, in some cases, kills them.”28
“Physicians working for the medical aid agency Médecins Sans Frontières [Doctors Without Borders] have saved limbs by applying sugar to wounds.”29
Studies and anecdotal reports from doctors show that when sugar (or honey) is applied to wounds, including burn wounds, the wounds heal without scarring, or with minimal scarring only.303132 It is suspected that sugar can prevent scarring because glucose is a building block for hyaluronic acid formation.33
Anyone who is even remotely into skincare knows that hyaluronic acid is the MVP (most valuable player) in the anti-aging and skincare world. The best skincare products contain hyaluronic acid, as it is known to keep the skin looking young and hydrated, increase skin elasticity and prevent wrinkles.
In inflamed tissues, scarring happens when the body is unable to regenerate healthy tissues and replaces them with fibrous collagen deposits instead. This inflammation causes tissues to produce excessive amounts of disorganized, fibrous collagen. While hyaluronic acid stimulates the synthesis of collagen, it stimulates its synthesis in an organized manner and prevents collagen over-production. It also lowers inflammation, which results in healthy skin regeneration, where the collagen adds to skin elasticity instead of making it hard and fibrotic.
Sugar has also been effectively used to treat wounds in diabetics,34 including diabetic foot ulcers.35
Sugar Is Liver Protective
Our liver’s key responsibility is processing various toxins that make their way into our bodies, including certain pharmaceutical medications, pesticides, environmental pollutants, estrogens, and glucocorticoids.
The liver processes substances in a two-phase manner. During phase 1 of liver detoxification, toxins are transformed to prepare them for elimination. This can temporarily make some of these substances more reactive and more toxic, which is why they have to pass through phase 2 liver detox, where they are made more soluble to make it easier for the body to excrete them.
To make toxins more soluble, in phase 2, they are combined with various molecules, such as glucuronic acid or amino acids. The most predominant of these combination (conjugation) reactions is glucuronidation, the combination of toxins with glucuronic acid. Do you know what glucuronic acid is derived from? Glucose.36
Very low carbohydrate diets have been shown to impair the clearance of drugs and toxins by the liver by depleting glucuronic acid.37 In other words, we know that glucose plays a fundamental role in allowing our liver to function correctly. Another fundamental way in which sugar supports liver function is by providing it with adequate energy. By doing so, pure sucrose (white table sugar) has been seen to lower liver inflammation and liver fibrosis, and to prevent the development of stress-induced fatty liver disease.3839
“The high sucrose diet had anti-inflammatory and anti-oxidant effects in the liver of animals with thioacetamide-induced cirrhosis. In addition, the high sucrose diet also improved malnutrition and catabolism present in cirrhosis. Thus, a high sucrose diet may be a therapeutic option for cirrhotic patients in a catabolic state.”40
It’s worth noting that in those studies in which sugar is seen to worsen liver health, animals are often placed on very high-calorie, high-fat, high-sugar diets, where the damage isn’t done by sucrose but by general overfeeding and the depletion of micronutrients needed for sugar and fat metabolism. It’s the general overfeeding which eventually causes the liver to start turning sugar into fat and can lead to fatty liver and related complications.
Alternatively, some animal models feed animals with pure fructose powder, exceeding their small intestine’s ability to absorb this fructose. This fructose then ends up feeding pathogenic gut bacteria, which, when overfed, can produce toxic byproducts, like endotoxin and even ethanol. These bacterial end products can then, in turn, hurt the liver.
Sugar Makes You Smarter
“The brain needs almost exclusively a constant supply of glucose from the bloodstream. Adult brain requires about 140 g of glucose per day, which represents up to a 50% of total carbohydrates consumed daily in the diet. The consumption of a food or beverage enriched with sucrose has been associated with improved mental alertness, memory, reaction time, attention and ability to solve mathematical problems, as well as a reduction in the feeling of fatigue, both in healthy individuals and patients with Alzheimer disease. An adequate nutrition of brain contributes to structural and functional integrity of neurons. It has been shown that in major mental illnesses such as schizophrenia, depression and Alzheimer's disease, nutritional deficiencies at cellular level are implicated.”41
Our brains are very sugar-hungry. The energy that brain cells derive from glucose is needed for their function, maintenance, and repair. Higher cognitive functions (studying, solving math problems, or playing chess) use up a ton of glucose.
Various studies found that when participants were given a mentally challenging task (testing for things like short-term memory, item location or immediate verbal recall), those given sugar performed better and were able to complete the task in less time.42
In one study, it was found that when elderly participants with mild memory complaints were given a drink with either 50 grams of pure glucose or 100 grams of sucrose, only the sucrose group showed improved attention and information processing speed.43 Honey, which contains free glucose and fructose as well as some sucrose, has also been found to prevent cognitive ageing and protect the brain from injury.4445
When a study in India46 measured the blood glucose levels and IQs of a cohort of healthy, male university students, those in the highest IQ bracket (with an IQ of 126-140) had higher insulin levels and higher blood sugar levels in the first 90 minutes after sugar ingestion. When blood sugar levels are maintained higher after a meal (given that the individual can efficiently use sugar for energy), the glucose in the blood will be prioritized for the brain. As such, based on this study, it seems that more sugar availability for the brain can result in (and be required by those with) a higher IQ. Blood glucose fell to baseline after 2 hours in all the IQ groups.

Sugar Supports Healthy Immune Function
Whenever we experience tissue damage or whenever we fall prey to a potentially pathogenic virus or bacteria, our immune system responds to fix the damage and prevent the proliferation of the infective agent.
Glucose is one of the major fuel sources that our immune cells use to power their function.47
It has been found that stressful exercise and overtraining depress immune function in humans, making them more prone to respiratory viral infections. Human studies found that eating sucrose (or carbohydrates in another form) before, during or after stressful exercise can offset stress-induced immune suppression and improve resistance to respiratory infections.4849
One mouse study50 found that when the animals were infected with a herpes virus, in the sucrose-supplemented group, fewer mice got sick, fewer died, and it took longer for symptoms to develop. This study tested both mice who were immunocompromised due to exercise stress (running on a treadmill until fatigued three days in a row), and those that were not subjected to exercise stress and were not immunocompromised. They found that both of the groups given sucrose, whether exposed to exercise or not, had a greater resistance to infection. This indicates that the immune system benefits of sucrose are not restricted to athletes/exercise stress.
Strenuous exercise increases the levels of stress hormones, such as cortisol and adrenaline, which have an immunosuppressive effect. By helping to dampen the stress hormone response and by providing fuel for different types of immune cells, sucrose has been shown to improve immune function.
“Substantial evidence in humans indicates that carbohydrate-containing sports drinks can offset the decreased immune function associated with stressful exercise. […] Carbohydrate containing sports drinks have received the most interest, largely for their ability to offset the exercise-induced alterations in immune system components via suppression of the stress hormone response.”51
What About Research Showing the Adverse Effects of Dietary Sugar?
There are a few problems with many of the studies that report on the adverse effects of sugar in the diet. These problems are:
Many epidemiological studies (studies where people are asked to complete surveys noting what they eat) lump poor quality diets consisting of ultra-processed long shelf life micronutrient void foods into the “sugar consumption” category.
Conclusions on the effect of sucrose consumption are drawn from studies designed in a way that doesn’t control for other variables and places subjects on high-sugar, high-fat, hypercaloric, and micronutrient-void diets.
Conclusions on human sugar tolerance are made based on rat and mouse models, which do not accurately represent human sugar tolerance.
Is Added Sugar “Bad,” But Natural Sugar “Good”?
Some epidemiological studies come out with results showing that sucrose from fruit is associated with positive outcomes, yet sucrose from processed foods isn’t. For example, this epidemiological study52 found that women who consume a lot of sugar from fruit are protected against preeclampsia but women who consume a lot of sugar from ultra-processed carbonated beverages have a higher risk of preeclampsia.
Studies which report findings in such a misleading way add to a phenomenon that I see far too often in social media discourse regarding nutrition. When I’ve spoken about the benefits of sucrose on my Instagram page, I’ve been asked to clarify “what I mean by sugar” since “sugar is good for you when it’s real sugar, like an apple, but not when it’s added white sugar.” However, that sentiment is incorrect.
Whether sucrose comes from an apple or white table sugar, it is the exact same molecule, meaning that sucrose is not the differentiating factor between the two groups in this study (or in any other similar studies that look at sugar intake from whole vs ultra-processed foods).
Rather, the participants who consume more of their sucrose from fruit and vegetables likely have access to higher quality (perhaps more expensive) foods and generally take their diet quality and health more seriously. On the other hand, those who get their sucrose from processed foods are more likely to have a lower quality micronutrient-void diet overall, perhaps because they are not health conscious or perhaps because fresh foods are unavailable to them, either because they live in a “food desert” or because they can’t afford them.
A more accurate representation of data would state that nutrient-void, ultra-processed diets create worse outcomes, as opposed to pretending that sucrose from fruit is different from sucrose from sugar. It isn’t, and it shifts the blame away from the true issue (an overall poor-quality diet) to a non-issue (whether or not the diet contains some sucrose). To circle back to the preeclampsia study, the ideal solution wouldn’t be to switch the women who drink ultra-processed carbonated drinks over to sugar-free versions of those drinks. The ideal solution would be to replace those drinks entirely with better quality carbohydrate sources, like fruit or fresh fruit juice, to make the diet more micronutrient-rich.
“In the case of table sugar or sucrose, it has been said that it is different to that found in foods which contain it, which is a clear error. Sucrose is a chemically pure substance which has only been separated from other components, which exists in the plant that it has been extracted from, sugarcane or beet, and is, therefore, identical to that which exists in the natural form in fruit. From a nutritional point of view, the only drawback that can be attributed to sucrose is that, as it is a chemically pure product it only provides energy and no other nutrients.”53
I understand that a layperson might be prone to falling prey to the belief that sugar in whole foods is different from purified sugar, as a basic understanding of biochemistry is needed to see that they’re the same molecule. However, the fact that some research publications report data in ways that perpetuate this misunderstanding is disappointing.
Diets high in “added sugar” are often found to be associated with worse health outcomes not because the sugar in candy is any different than that in oranges, but because oranges have more vitamins and minerals. Lack of micronutrient density, and diets full of low-quality, hyperpalatable, ultra-processed foods, as opposed to sugar, are the true crux of the problem.
Hypercaloric, High Fat, High Sugar, Highly Processed Diets are Not “High Sugar Diets”
The majority of studies reporting on deleterious effects of high sucrose diets tend to place study participants (or study animals) on high sucrose, high fat, high calorie, micronutrient-void diets.
In these scenarios, multiple factors are being changed, and the study design is not controlling for just the increase in sucrose on an otherwise healthy diet. Diets that are high in fat interfere with the utilization of sugar for energy (something that I will talk about later in this article and something that I discuss in more detail in my diabetes article), so a diet that is both high in fat and high in sugar (the Western diet) will almost always produce bad outcomes. On such diets, the damage is mostly done by the general overfeeding (past the test subject’s caloric maintenance) on nutrient-void foods, eventually depleting the micronutrients needed for sugar (and fat) metabolism, and causing the test subject to put on body fat, which increases the levels of fat in the blood and further interferes with glucose metabolism.
Similarly, when studying groups of people who follow different diets, those who eat a high-calorie, ultra-processed, high-fat, high-sugar Western diet are often grouped into the “high-sugar diet” category, even though, in reality, an average vegan or vegetarian might be eating more sugar than they are.
As yet another confounding variable, studies where sucrose is added to an otherwise healthy diet are rarely conducted. Instead, the studies are either done on humans eating the Standard American Diet (as already mentioned), or on animals which are force-fed an excessive amount of sugar. While these studies claim to be testing for the negative effects of sugar, in reality, they are testing for the negative effects of overfeeding.
Generally, studies done on humans where calories aren’t increased and where sucrose is substituted for starch in a calorie-for-calorie manner do not show adverse effects (or any difference between the two, really). Additionally, oftentimes, when sucrose is increased on a diet that is low to moderate in fat and adequate in vitamins and minerals, there are improvements in health markers.54
“We systematically reviewed interventions substituting sucrose for other macronutrients in apparently healthy adults to assess impact on cardiometabolic risk indicators. […] There was little evidence for significant effects on plasma glucose or insulin. Sucrose substitution for starch up to 25% energy does not appear to have adverse effects on cardiometabolic risk indicators in apparently healthy adults.”55
“Sixteen well-controlled type II diabetic subjects were fed three isocaloric diets for 28 days each. […] When consuming a diet with nearly 60 g/day of fructose (20% of the total calories) for 28 days, our patients had a glycemic control and lipid profile indistinguishable from those observed with a control starch diet. Indeed, the small, nonsignificant, reduction in postprandial glycemia with the high-fructose diet might even suggest a trend toward an improved glucose metabolism.”56
Rodents Have a Lower Sugar Tolerance Than Humans
Data from rat and mouse studies is often used to infer the potential risks or benefits that a certain dietary approach may have on humans. While this works out great most of the time (since rodents are similar enough to us, and since many of the studies that we can do on animals would be highly unethical if done on human subjects), mice and rats have a far lower sugar tolerance than humans. Humans have a better sugar tolerance than rodents mostly because of our large, sugar-hungry brains.57 Our threshold for sugar is a lot higher than that of rodents, as our tissues have a greater need for it. Humans can shuttle a lot of sugar towards energy generation. Rodent tissues have a lower need for sugar, so reaching an excess of sugar isn’t difficult in rodents. Rodents start to convert sugar into fat (fuel for later) at a much lower threshold.58
Consequently, we can’t always get accurate data on human sugar tolerance from animal models.
All in all, whenever all other factors are controlled (calories, fat intake, micronutrients) and sucrose is added in place of other carbohydrate sources (or is added to an otherwise healthy diet), we do not see test subjects getting violently ill, becoming poisoned, experiencing extremely out of whack blood labs, or any other symptoms that would unanimously back up the “sugar is the white death” claims.
Busting Sugar Myths and Misconceptions
After reading this, most of you might still have concerns regarding sugar, such as:
Doesn’t it cause high blood sugar levels?
Doesn’t it cause insulin resistance?
Doesn’t it feed cancer?
All of these concerns (and more) will be covered and debunked in this section.
Sugar Isn’t the Cause of High Blood Glucose Levels
I go over this topic in detail, and with many research references, in my diabetes article and in this podcast episode that I did on blood sugar balance, so check those out for a deep dive into this topic. In the meantime, here are the cliff notes.
Blood is a “highway” of sorts, meant for delivering fuel (in the form of fats or glucose) and micronutrients to our cells. Even if we were to eat absolutely zero sugar (as in the case of the zero-carb carnivore diet), there will always be glucose in our blood. When we don’t eat any carbs, the liver will produce glucose out of proteins and fats to maintain blood glucose levels (this process is called gluconeogenesis).59
In diabetics, high blood glucose is mostly caused by the liver overproducing glucose out of non-carbohydrate sources, paired with cells that struggle to burn glucose well. The overproduction of glucose by the liver is usually caused by high levels of our main stress hormone, cortisol.60 Cortisol levels can be excessively high due to underlying low thyroid function, psychological stress, overtraining, fasting, or low-carb diets.
“Increased gluconeogenesis in the liver of patients with type 2 diabetes is considered a major contributor to hyperglycemia and subsequent diabetic organ damage.”61
The body will always be producing glucose because many of our cells (especially those making up the brain and nervous system) rely entirely on glucose as a fuel and cannot fully switch to burning either fats or ketones for energy.62 A steady supply of glucose in the blood (whether it comes from dietary glucose or the liver converting proteins or fats into glucose) is necessary to keep the nervous system and brain functioning. If blood glucose drops too low, a person can get aggressive and belligerent. If it drops even lower, they lose consciousness. Even lower and they die. In short, whether or not you eat carbs, unless you are dead and decomposing, you will always have glucose flowing through your blood.
While the idea that high blood sugar is caused by eating sugar is appealing, this idea falls apart when we realize that:
The liver creates sugar out of non-sugar sources in stressful conditions (under the influence of the hormone cortisol).
Physiologically, carbohydrate avoidance is a stressor (it increases cortisol levels, as cortisol is needed to make glucose when none is eaten).63
Eating carbs (especially sweet-tasting ones) lowers cortisol.64
When there is nothing interfering with our cells’ ability to burn glucose, blood glucose levels remain in range and rarely “spike,” or get high.
For glucose to spike and/or to remain steadily elevated in the blood, a few different metabolic mechanisms must go awry in the background. However, none of these “metabolic breakdowns” that interfere with the burning of glucose for energy are caused by glucose (sugar) itself.
Usually, glucose builds up in the blood when:
The liver is overproducing glucose under the influence of cortisol.
There is too much fat in the blood, resulting in cells excessively taking up and burning fats for energy, which prevents them from burning glucose for energy. Any cell can only burn either glucose or fat at any given time, and if it’s burning fats for energy, it can’t simultaneously burn glucose for energy. This can be due to a diet that’s both high in carbs and fat, or due to high cortisol and adrenaline levels, as high cortisol and adrenaline levels liberate fat from fat stores into the blood.
Glucose enters the cell but fails to enter cellular respiration (the process of turning glucose into cellular energy, which consists of three stages: glycolysis, the Krebs cycle, and the electron transport chain), so it flows back out of the cell and into the blood.65 This happens when:
Cofactors for cellular respiration are lacking, resulting in blockages somewhere along the respiratory chain. This blockage can be due to a deficiency of one or more of the cofactors needed for glucose metabolism, such as magnesium, biotin, thiamine, or copper, among others.
Oxygen levels in the cell and/or intracellular thyroid hormone levels are low. The shortage of oxygen and thyroid hormone can impair/slow down cellular respiration, preventing more glucose from being oxidized.
Certain toxins (such as high nitric oxide levels) can block parts of mitochondrial respiration. High oxidative stress (which is amplified by the presence of toxic metals and the incorporation of unsaturated fats into cellular components) can also cause respiratory blocks and impair glucose oxidation.
“The block occurs ‘lower down’ in the metabolic pathway. […] Under these conditions, glucose […] is effectively blocked at the entry point to the Krebs cycle by the excess of metabolites arising from fat and protein breakdown. […] As a result, much of the ‘free’ intracellular glucose transported into the cell is transported back out of the cell into the extracellular fluid.”66
The lack of vitamin and mineral cofactors for sugar metabolism is often the biggest part of the high blood glucose problem. Vitamin B1 (which is needed to burn sugar for energy and helps pyruvate, the breakdown product of glucose generated during glycolysis, enter the mitochondria) and magnesium (which is also needed to burn sugar for energy and helps pyruvate enter the mitochondria) have both been successfully used to lower blood glucose levels and reverse diabetes type 2.6768
My article going into nutrients that help to combat type 2 diabetes goes into more detail as to how different vitamin and mineral cofactors affect glucose metabolism.
As shown, the main offenders contributing to high blood sugar levels are:
High-calorie malnutrition (the lack of vitamins and minerals needed for carbohydrate metabolism in the diet, such as vitamins B1, B3, B5, B7, chromium, magnesium, copper, and zinc)
Undiagnosed hypothyroidism (potentially caused by a deficiency of the mineral and vitamin cofactors needed to make thyroid hormones, such as selenium, iodine, and retinol)
Psychological & physiological stress
High free fatty acids in the blood, either from the overconsumption of fat, from being overweight or due to the liberation of fat into the blood under stress
Pollutants and endocrine-disrupting chemicals, including toxic metals, such as mercury, which can lower thyroid hormone levels, hurt the structure of cells and interfere with parts of cellular respiration
The best way to avoid high blood sugar levels is to be good at burning sugar. Being bad at burning sugar, the preferred form of fuel for our cells, is a sign that there are issues with our cellular and metabolic machinery which need to be addressed to “unblock” our ability to burn glucose well. Addressing our micronutrient status, macronutrient ratio, stress levels, meal frequency (to avoid long periods without meals and to avoid over-eating at one meal and under-eating at another meal), thyroid health, exposure to pollutants, avoiding a chronic caloric surplus (and finding your maintenance calories instead) and not being sedentary are the main pillars to focus on to fix this. Something as simple as walking can increase the number of receptors that take up glucose on cell membranes, helping to get glucose into cells and out of the blood.69
Long term, switching to a high-fat, ketogenic diet and avoiding carbohydrates (sugar) makes us worse at burning sugar for energy - not better, which is a problem since…the body will always make sugar. This is explored in my article on diabetes.
Sugar Isn’t the Cause of Insulin Resistance
Insulin’s main role is colloquially believed to be to push glucose into cells. This view of insulin is stated in many health outlets which claim that insulin is required for cells to take up glucose and insist that, since insulin is released whenever carbohydrates are eaten, if you eat carbohydrates often and release insulin often, your cells will eventually “get tired” of responding to insulin. They will become “resistant” to its call. As a result, they will stop taking up glucose, leaving it high in the blood.
While on a surface level this explanation might make sense, we now know that of the 14 known transporters that cells use to take up glucose, only two are regulated by insulin.
Cells take up glucose and fructose using transport proteins called GLUT. There are currently 14 known GLUT proteins, aptly numbered 1-14. The first five (GLUT1-GLUT5) are the most studied.
Of the 14 GLUT transporter types, only two are known to have a strong relationship to insulin: GLUT4 & GLUT12.70 Of the two, GLUT4 is the more abundant and better-studied transporter. This transporter exists in muscle, fat and liver cells. However, insulin doesn’t cause GLUT4 to take up sugar. It simply calls more GLUT4 receptors to the cell membrane, where they can act as doors for glucose to enter the cell. It has the same relationship to GLUT12.
“Insulin stimulates the translocation of a pool of Glut4 to the plasma membrane.”71
The often presented picture of insulin is as pushing glucose into the cell. In reality, insulin doesn’t push glucose into the cell but rather creates more opportunities for cells to take up glucose. If we think of the GLUT4 transporter as a door through which glucose can enter the cell, insulin doesn’t push glucose through this door. It prompts the appearance of more doors but doesn’t control glucose’s entry through them.
What is especially ironic here is that fructose (which is part of sucrose and “sweet tasting” carbohydrates) doesn’t stimulate the release of insulin. Fructose is absorbed through GLUT5 and GLUT11 transporters. After being taken up by the liver, the liver converts fructose into glucose and slowly releases it into the blood.
So, is insulin’s job to call upon more doors that cells can use to let glucose in? That’s part of it. However, apart from calling in more GLUT4 transporters, insulin’s other roles are to:72
Stop the liver from producing sugar.
Stop the release of fats into the blood.
Since most GLUT transporter types are insulin-independent, we can conclude that insulin’s main role in the body has more to do with “switching off” the “backup generators” when fuel comes in. This is why, when we eat carbs, insulin tells the liver to stop producing sugar and tells fat cells to stop releasing fat into the blood.
Adaptive vs. Pathological Insulin Resistance
There are some instances in which, despite carbohydrates being consumed and insulin being released, cells are unable to respond to insulin. When this happens, the liver keeps making sugar despite dietary sugar coming in, fat cells continue to release fat into the circulation (despite insulin being there telling them to stop), and GLUT4 transporters fail to migrate to the cell membrane. This is what insulin resistance really looks like.
Is sugar consumption what causes this? No.
Sometimes, insulin resistance can be adaptive. Often, this adaptation takes place under stress, when various signalling molecules tell the body that the demands placed on it exceed the energy supply from food.
For example, let’s say that the amount of carbs coming in from the diet at any given moment is too little to meet the requirements of your glucose-requiring tissues. An example of this might be a time when your brain (a glucose-dependent organ) has to work extra hard (let’s say, you’re studying for an exam). Dietary glucose might not be enough to meet your brain’s needs when more demands are placed on it, so despite insulin’s signal which says “Hey, we have fuel coming in, turn off the backup generators!” the body chooses to keep the backup generators running, as the fuel coming in isn’t enough on its own to fulfill the increased needs of the brain at this time. This sort of adaptive (healthy) insulin resistance was seen in the earlier-mentioned study on Indian university students, where those with higher IQs seemingly had brains with a higher glucose requirement, and, with their bodies using adaptive insulin resistance (prioritizing fat burning in muscles and other tissues), more glucose was spared for the brain.
In adaptive insulin resistance, by choosing to continue producing its own sugar (despite sugar coming in), while also releasing fats into the blood and reducing the expression of GLUT4 in the cell membranes of muscle cells, the body forces cells which technically can run on fats to run on fats, while sparing glucose for the brain.
Other examples of “energy demand exceeding energy supply” in which the body can choose to become insulin resistant as a protective mechanism to ensure that cells can get the energy they need to overcome a stressor are infections, pregnancy, and fasting.
However, usually, when discussing insulin resistance, we are talking about pathological insulin resistance. While adaptive insulin resistance is meant to be protective in the face of acute stressors, pathological insulin resistance happens in response to chronic stress.
As mentioned, the signalling molecules that tell the body to become insulin resistant as a protective mechanism are elevated under stress. However, “stress” can be many different things. An acute stressor could be a respiratory infection. Suffering from a respiratory infection can elevate certain inflammatory mediators that tell the body to become insulin-resistant to prioritize a steady supply of glucose for the immune cells fighting an infection until the infection is overcome.
But what happens when these inflammatory mediators are chronically, and not acutely, elevated? Gut dysbiosis, bacterial overgrowths in the gut, untreated chronic infections, high levels of oxidative stress (oxidative stress is amplified in the presence of toxic metals and unsaturated fats), air pollution/cigarette smoke, and even the presence of too much fat on the body all result in the release of those same inflammatory mediators! This can make the insulin-resistant state chronic and pathological. For the nerds reading this who might want to know the specific signalling molecules that interfere with insulin’s signalling, they are NF-κB, JNK, TNF-α, IL-6, and TLR4.
Cortisol itself, the main hormone elevated under stress, can block insulin’s calls.73 Cortisol and insulin send opposing signals, and they play a sort of tug of war with one another.
Cortisol tells the liver: “Make more sugar.” It also tells fat cells: “Release fat into the blood!” Insulin tells the liver: “Stop making sugar” and tells fat cells “Stop releasing fat into the blood!”
When cortisol is too high, it can muffle the signal sent by insulin.
As mentioned, cortisol is an adaptive hormone, meant to elevate in times of acute stress (when fasting, for example) to make sure that blood sugar never falls too low. However, hypothyroidism, psychological stress, high estrogen levels, infections and even gut dysbiosis can cause cortisol to remain chronically elevated even when food is coming in.
“In primitive man, the stress response mechanism was acutely activated by physical stressors and led to insulin resistance and mobilization of energy to be used for an adaptive response. In today's society, chronic activation of the stress system by psychosocial stress leads to inappropriate induction of insulin resistance.”74
Additionally, when cells are excessively relying on fat burning for energy, this can inhibit the migration of GLUT4 receptors to cell membranes.75 After all, it makes sense. If the cell is already burning fats, it will not want to take up glucose, since it can only burn one fuel type at a time. Cells are more likely to switch to burning fats for energy either when fats are very abundant in the blood or when the cofactors for glucose burning are missing, so they have to burn fat. (By the way, fat also needs cofactors to be burnt for energy, vitamin B2 being an important one).
In summary, insulin resistance is the consequence of chronic inflammation, chronically high cortisol levels (chronic stress) and excessive reliance on fat burning, all of which block insulin signalling. In a few instances, low-fat, high-carbohydrate diets have been shown to ameliorate insulin resistance by lowering cortisol and lowering the competition between blood sugar and blood fats. Antibiotics have also been used to resolve insulin resistance, as have other approaches to modulating the microbiome and clearing gut and systemic infections.76 This is something that I’ve already talked about in more detail in my diabetes and glycation articles.
The goal here isn’t to defend sugar at any cost. However, since the body will always produce and use its own sugar (even in the total dietary absence of sugar), it’s clear that insulin resistance can’t be solved by avoiding sugar. This is made even more clear by many of those who start pursuing a zero-carb diet, only to eventually experience increases in their insulin and blood sugar levels…despite eating zero sugar. Clearly, the issue here is deeper, and it’s these deeper layers that need to be addressed to solve the problem at its root.
Sugar Doesn’t Damage Your Metabolism or Cause Inflammation
Honestly, both of these statements are used in extremely vague ways both in online discourse about sugar and in most health books, so it’s difficult to gauge what statements like “sugar damages the metabolism” or “sugar is inflammatory” are referring to.
Here is, however, what we do know for sure about sugar, the metabolic rate and inflammation.
All of our cells need adequate cellular energy to maintain their structure, function, maintenance and repair. If a cell can’t make energy, it dies.
There are two substrates out of which cells can make this energy: glucose or fats.
When cells struggle to generate adequate energy at a rate that is rapid enough and fail to meet their energy needs, disease states manifest. To create this energy in a way that is rapid and complete, apart from adequate micronutrient cofactors, cells also need enough thyroid hormone (it controls the speed at which cellular energy is made) and enough intracellular oxygen (without which energy cannot be generated).
Low carbohydrate diets lower thyroid hormone levels and slow down the rate of metabolism.77 Higher carbohydrate intake increases thyroid hormone levels and accelerates the rate of metabolism. Additionally, burning glucose for energy (as opposed to fat) generates more cellular energy per unit of oxygen and helps to get more oxygen into the cell.7879 In short, it’s carb avoidance that lowers the metabolic rate or “damages the metabolism.”
As per “inflammation,” chronically high blood glucose levels can be inflammatory, since, to achieve equilibrium, the body will start using alternative pathways to dispose of excess glucose when it fails to use it. These backup pathways aren’t very efficient and often increase oxidative stress. I talk about this in my glycation article.
However, as established earlier, it’s possible to have high blood glucose levels even when eating zero carbs, in instances where chronic stress and other factors stop insulin from telling the liver to stop making glucose, and when cells are unable to completely and effectively metabolize glucose. Cells’ inability to metabolize glucose fully can be caused by, as mentioned earlier:
A deficiency of one or more of the nutritional cofactors for any stage of cellular respiration (the process of cellular energy generation).
High levels of fats in the blood
Chronically high cortisol levels
Low thyroid hormone levels
Low levels of intracellular oxygen
Chronic inflammation from gut dysbiosis or bacterial overgrowths (bacterial toxins can increase inflammatory mediators that block parts of mitochondrial respiration)
Pollutants and endocrine-disrupting chemicals, including toxic metals, such as mercury
The intermediates created from glucose metabolism when glucose fails to be metabolized completely can also be inflammatory. For example, after passing through glycolysis (the first part of cellular respiration), if pyruvate, generated from glucose during glycolysis, fails to enter the Krebs cycle (either due to blockages further up in the electron transport chain or due to a deficiency of an important Krebs cycle cofactor, such as B1), it gets turned into lactate instead. Lactate can be pro-inflammatory.80 However, again, the glucose isn’t the issue. The real issue(s) are the factors that inhibit cells from burning glucose rapidly and completely.
When cellular respiration happens too slowly, this can increase oxidative stress, which increases inflammatory mediators which then result in high blood sugar levels. Again, eating carbohydrates (sugar) isn’t what causes this. It’s the factors above.
Since this section just skims the tip of the iceberg on topics such as thyroid health, metabolism, and how adequate cellular energy is a requirement for good health, check out my other articles going into these topics for far more information (and the supporting research and literature). My articles on the bioenergetic view of health (Dr. Ray Peat’s work), diabetes, glycation, hypothyroidism, PCOS and heavy metals go into these topics in more detail.
Sugar Doesn’t Cause Cancer or Diabetes
While the above three sections talk about the myriad of factors that contribute to insulin resistance and high blood sugar levels, I think that the most convincing piece of evidence (one that doesn’t look so closely at the biochemical pathways) comes from the work of those like Dr. Walter Kempner who managed to bring diabetes to remission (and get obese subjects to lose tremendous amounts of body fat) on diets of basically just white rice, white sugar, fruit and juice. I do not think that such a diet is optimal for anyone (for many reasons), but it does make you go “hmm” about the long-accepted adage that it is sugar which causes diabetes. I cover Dr. Kempner’s work in my article on diabetes.
“Sugar feeds cancer” is another statement which often gets repeated and reiterated everywhere. First, a reminder that even if we eat zero carbs, we will always make glucose which can be supplied as fuel to all cells (including cancer cells).
In my article “Cancer Can Thrive on Fat” I go over research showing that cancerous cells can, and do, use fat as a major fuel source (they use protein and ketones too). In short, it’s impossible to selectively “starve” cancer cells without starving and depleting ourselves, which will only further many of the metabolic derangements seen in cancer. The metabolic derangements brought on by various environmental factors which lead cells to turn cancerous and turn on the expression of cancer genes are the crux of the problem to be addressed. This is something that I explored in far more detail in my two articles diving into the topic of cancer, including my other article: “Cancer: Metabolic or Genetic?”
The perception of “cancer feeding on sugar” comes from the fact that cancer cells do take up glucose at a rate that exceeds that of normal cells. However, cancer cells are characterized by impairments in cellular respiration which prevent them from creating adequate cellular energy (ATP) from fuel sources. Most of the glucose that enters cancer cells isn’t fully oxidized but turned into lactate instead, a phenomenon called The Warburg Effect. In other words, cancer cells take up a lot of glucose but they can’t use it well and waste most of it.
“In contrast to normal differentiated cells, which rely primarily on mitochondrial oxidative phosphorylation to generate the energy needed for cellular processes, most cancer cells instead rely on aerobic glycolysis, a phenomenon termed ‘the Warburg effect.’ Aerobic glycolysis is an inefficient way to generate adenosine 5′-triphosphate (ATP) […] The metabolism of glucose to lactate generates only 2 ATPs per molecule of glucose, whereas oxidative phosphorylation generates up to 36 ATPs upon complete oxidation of one glucose molecule”.81
An analogy here would be someone with collapsed lungs gasping for air. They are taking more breaths than the average person, creating the illusion of breathing more oxygen, even though they’re failing to actually get oxygen into their lungs. The solution isn’t to block their ability to gasp for air but to address their lung condition and restore their ability to take a full breath.
Glucose avoidance increases the expression of AMPK. AMPK is akin to an alarm bell that goes off when cells don’t have enough cellular energy (ATP) to meet their needs, or when glucose levels are low.
“AMP-activated protein kinase (AMPK) is a highly conserved sensor of low intracellular ATP levels that is rapidly activated after nearly all mitochondrial stresses.”82
“The canonical role of AMPK is in monitoring cellular energy status by sensing the levels of AMP and ADP relative to ATP […] AMPK is also activated by glucose deprivation […] This mechanism can occur in the absence of any changes in AMP/ATP or ADP/ATP ratios.”83
AMPK is elevated in most cancers, due to the inhibitions in cellular energy generation seen in cancer. However, the signalling of AMPK also promotes certain pathways which further cancer progression, making high AMPK a cancer promoter.
“AMPK could elicit numerous oncogenic mechanisms to promote cancer progression and metastasis, offering potential therapeutic strategies to target AMPK pathways for cancer treatment.”84
“High AMPK activity in low adhering migratory cells, induces mitochondrial fission, resulting in lower oxidative phosphorylation and lower mitochondrial ATP. […] AMPK inhibition suppresses metastatic potential of amoeboid cancer cells in vivo.”85
In short, glucose deprivation (since it is a stressor) could accelerate cancer progression, something that I cover in the above-mentioned articles exploring the metabolic roots of cancer.
Sugar Doesn’t Cause Glycation and High HbA1C
Advanced glycation end products (AGEs) are a class of molecules capable of damaging proteins, such as collagen, impairing their function and elasticity. AGEs activate a variety of metabolic pathways that can impair cells’ ability to make energy, increase oxidative stress, and even cause cell death.
Glycation is what is measured by the popular HbA1C blood test, and when the test comes back high, it can be bad news.
Since glycation can accelerate skin aging, sugar is often said to “age the skin,” even though, as mentioned earlier, glucose is a precursor to the skin-regenerating hyaluronic acid. Glucose is also not a very good glycating agent!
While sugar is often painted as the villain when it comes to glycation, glycating agents are derived from metabolites of carbohydrates, proteins, fats, and ketones. While glucose itself is a poor glycating agent, the breakdown products of glucose (which accumulate when cells have a hard time metabolizing glucose) are much more likely to be implicated in glycation. Once again, since the body will always make glucose no matter what, avoiding dietary carbs won’t fix this. Fixing impairments in glucose metabolism will fix this. Additionally, the glycating agents derived from ketones are more damaging than those derived from glucose. Lastly, AGEs aren’t just something that we produce in our bodies. A lot of AGEs enter our bodies from improperly prepared foods. I talk about this topic extensively in my two-part deep dive into glycation:
When it comes to preparing cooked foods in ways that minimize glycation, white table sugar is a lot less glycating than corn syrup, agave syrup or even honey. This is because the glycosidic bonds holding the glucose and fructose together in sucrose molecules prevent these sugars from reacting with proteins. This too is covered in more detail in my glycation series.
Sugar Isn’t “Empty Calories”
By definition, a calorie cannot be empty. Calories are a way to measure the energy content of food. Would the sentiment still make sense if we called it “empty energy?” Not so sure about that.
Sugar (glucose) is the preferred source of energy for our cells, and when it is added to foods, it is simply a source of extra energy. Would it be better if our sugar source also came with cofactors needed for sugar burning, such as magnesium, B1 or copper? Of course. However, the body always has some amount of these micronutrients stored (this is why deficiencies take time to develop), and can use them to burn the provided fuel source for energy.
If a person relies on refined sugar sources for most of their energy intake, they will likely develop deficiencies over time. But did you know that Beri-beri, the disease of B1 deficiency, was first observed among populations eating heaps of white rice? Yup, it wasn’t observed among people adding a few sugar cubes to their coffee. When’s the last time someone shamed you for eating white rice, calling it empty calories? There’s as much sugar in a 200-gram serving of boiled white rice as in around 13 teaspoons of white table sugar.
“Beri-beri is a disorder of nutrition, and as it occurs in this country is associated with a diet in which white rice is the principal constituent.”86
As dietary staples, micronutrient-rich sugar sources (such as fruit, potatoes and other tuberous vegetables) are preferred, but it’s not because the sugar in them is any “different” but because they provide the vitamins and minerals needed for sugar burning.
By adding some sugar to your coffee, oatmeal or tea, you are not adding “empty calories.” You are just adding some more fuel to your food, fuel that the body can make energy out of. Again, the energy that your cells can make out of this fuel is the energy that they need for their function, structure, maintenance, repair, and even cell-to-cell communication. There is a reason why athletes often use sucrose tablets (yes, literally sugar in a pill) to maintain their energy during exercise. The practice of taking sucrose tablets is especially popular among long-distance runners.
We don’t call rice or refined wheat empty calories, even though they lack mineral and vitamin cofactors just the same as white table sugar. We also don’t call added fat “empty calories,” even though fat on its own lacks the cofactors needed for fat burning (such as carnitine and the B vitamins). No one freaks out if someone eats rice or adds some coconut oil to their meal, calling it “empty calories.” Why sugar then?
Calories aren’t empty. They provide our bodies with energy and keep us alive.
Sugar Isn’t Something That Only Young, Lean People Can Eat
“You can only eat sugar when you’re lean and metabolically healthy. When you’re older, you can’t have sugar” - is a sentiment that I’ve seen multiple times online.
It is true that in cases of all metabolic diseases (hypothyroidism, diabetes, cancer), cells’ ability to burn glucose effectively is impaired. However, since, as mentioned multiple times in this article, the body will always produce glucose, there is no way to sidestep this issue without solving it. The way to solve this issue is to restore proper metabolic function, by repleting micronutrients (including the vitamins, minerals and amino acids needed to make thyroid hormones), lowering stress, addressing gut dysbiosis, lowering estrogen levels, addressing environmental pollutants, finding one’s maintenance calories, and finding a balanced macronutrient split.
Fixing one’s metabolism can’t be done overnight, and if someone comes from a background of chronic illness or is currently in menopause, doing so will be tougher and take longer. Still, it is the only solution, since glucose in the body cannot be avoided, and avoiding dietary carbohydrates (including simple sugars) only makes us worse at burning glucose for energy.
Also, although I understand that saying this can be taken as survivorship bias, there is a reason why many centenarians list chocolate, and not kale, as a daily staple in their diets, and why they attribute their longevity to their sweet tooth.
Sugar Isn’t Addictive
“The idea of some ‘experts’ that sucrose can provoke some form of addiction in the same way as illegal drugs and, therefore, should be included in the list of addictive substances, is an opinion that has little scientific proof. The experimental evidence does not support the claim that sugar and other highly palatable foods produce addiction. It is important to qualify that sucrose forms part of foods that produce pleasure but not dependence.”87
Those who decide to go faux “sugar-free” (by cutting out candy, chocolates, and other sweet foods that they tend to snack on in between meals or when bored) often find that their sugar cravings become stronger after doing so. This gets attributed to so-called “sugar addiction,” and those who experience this equate it to a drug withdrawal.
The hunger and cravings experienced by those who cut out sweet foods aren’t a sign of addiction whatsoever. Rather, by cutting out sweet snack foods, a person often ends up unintentionally putting themselves in a caloric deficit, often a steep one. Their sugar cravings are the body saying “Hey, I need more energy! I am used to running on 2,000 calories a day and you just slashed them down to 1,400 overnight!”
The reason why the cravings tend to go away after a few weeks is that the body eventually adapts to the lower caloric intake by lowering the metabolic rate, making 1,400 calories its new maintenance. This is called metabolic adaptation. If the body were to continue expanding 2,000 calories per day while only given 1,400, it would eventually waste away and die. To prevent this from happening, the body downregulates its metabolism, slowing down its various functions and deprioritizing others. This is why many of those who “cut out sugar” might find that at first they lose fat, but eventually start to experience problems with hair loss, constipation, low energy, or feeling more depressed. These symptoms are not signs of sugar withdrawal. A sugar “withdrawal” is impossible since the body always makes sugar. They are signs of a slowing metabolic rate, from a diet that’s too low in calories for the person’s needs.
The statement “sugar lights up the same parts of the brain as cocaine” is still repeated into oblivion as some stone-cold truth by every self-proclaimed health guru. None of them seem to stop and think “Hm, maybe it’s the other way around? Maybe a more accurate statement would be ‘cocaine lights up the same parts of the brain as our body’s preferred fuel source,’” since, you know, our bodies evolved along glucose and not cocaine.
The reason why sugar lights up the so-called “pleasure centers” of the brain is because these centers are used to encourage the body to do things which are beneficial for it. Such as obtaining fuel, which keeps the body alive. When you eat something that contains sugar (fuel, potential cellular energy), the “pleasure centers” light up as the body’s way of saying “Hey, fuel keeps me alive and I like staying alive. Keep going.”
Additionally, let’s also point out that there is no such thing as a “pleasure center” in the brain. Sugar and cocaine both seem to have an effect on dopamine, in different ways. While dopamine is often associated only with pleasure and reward, it is also an important neurotransmitter for focus, memory, coordination, and social engagement. Cocaine prevents the reuptake of dopamine and adrenaline, increasing dopamine and adrenaline levels. It also acts on other neurotransmitters, for example, blocking acetylcholine receptors. On the other hand, sugar simply causes a dopamine release.
The body releases dopamine in response to sugar, partially because fuel is good for us, and partially because sugar increases the metabolic rate and lowers cortisol. Chronic stress8889 and a low metabolic rate90 (and the high cortisol levels seen in both of those states) lower dopamine. Adequate levels of dopamine are paramount to maintaining a healthy brain, with low dopamine being a contributing factor to Parkinson’s and dementia. Drug cravings and dependency are often the body’s misguided attempts at trying to restore a biochemical equilibrium. They are misguided attempts at meeting the body’s needs which fail to actually meet those needs.
For example, those who develop an alcohol dependency are often anxious and have low GABA levels. Alcohol stimulates GABA receptors. However, it doesn’t address the physiological problem: GABA levels being low and stress hormones being high, contributing to anxiety. Increasing the intake of nutrients that help to make GABA (such as magnesium and vitamin B6), and lowering the levels of cortisol and adrenaline by eating enough calories and improving thyroid function would be what would have to be done to address the physiological imbalance that pushes people towards their drug of choice: alcohol.
A person who is chronically stressed and hypothyroid might crave a dopamine-agonist drug because their dopamine levels are low as a result of their metabolic state. The correct solution here isn’t to take a dopamine agonist but to fix the underlying state of chronic stress and low metabolism. Sugar can help achieve this.
Additionally, anyone who has ever spoken to someone who has gone through an actual withdrawal, whether it be from alcohol or hard drugs, will know that becoming hungry and a bit grumpy is not at all equivalent to a real withdrawal. When a person stops eating sweet foods, or even if they go keto, they don’t actually “withdraw” from sugar. Their liver keeps making sugar, as otherwise they would die.
In a real withdrawal, neurotransmitter levels and their receptor expression are often extremely altered. The body always seeks equilibrium and in cases of drug addiction, the body tends to downregulate the receptors corresponding to the incoming substance. For example, within four weeks of going on some SSRIs, the brains of those given certain SSRI drugs downregulate the expression of serotonin receptors, making their brains less sensitive to serotonin. Now, if they stop taking the drug abruptly, their brains no longer express enough serotonin receptors to respond to the physiological levels of serotonin present in the absence of the drug. If such a change is done abruptly (whether the drug in question is a prescription drug, such as SSRIs or benzodiazepines, alcohol, or a “street drug” like heroin) the withdrawal can result in agonizing pain, inability to function, psychosis and even death. Anyone who equates the peckishness they might experience when they cut out candy to a drug withdrawal is almost offensively ignorant of the grim reality of drug dependency and addiction.
Speaking as someone who has fallen prey to believing the “sugar is addictive” fallacy in the past, imagine my surprise when…my sugar craving disappeared entirely when I started eating more calories, stopped restricting carbohydrates (including simple sugars, like fruit juice, honey, maple syrup or white sugar in my coffee), started meeting my micronutrient needs, and, in other words, started meeting my body’s energy requirements. Back in my paleo days when I believed that “sugar is poison,” it took me insane amounts of restraint to not want to binge on Oreo cookies or other ultra-processed sugar-containing junk that someone placed in front of me. I would nearly shake looking at them, as my poor body was screaming “Dude, this right here is energy! You need energy! Your ‘healthy diet’ has made you so malnourished that your period disappeared.” Nowadays, I couldn’t care less when around conventional sugar-containing junk food. I do not crave it, I do not want it, and if ever offered some, I happily deny it. If I ever do have a conventional sweet snack, I do not crave seconds (whereas in the past, if I had one cookie, I would have an insanely hard time preventing myself from eating the whole pack). Sugar addiction isn’t real. Malnutrition is.
Lastly, for anyone who is still adamant about believing that sugar will always make a person overeat and lead to “food addiction” because it is hyper-palatable, I invite you to open a bag of white table sugar and try just eating it with a spoon. How many spoonfuls can you eat before you realize that sugar on its own isn’t hyper-palatable and isn’t pleasant to eat? Probably not that many. While it is true that many ultra-processed foods are engineered to make them hyper-palatable, it’s not sugar on its own that makes them so. Rather, flavour enhancers, artificial flavours, “proprietary manufacturing techniques,” and a mixture of both fat and sugar contribute to the creation of foods that taste as if they were micronutrient-dense (hence the hyper-palatability) while providing little nutritional value.
Sugar Doesn’t Cause Cavities
“Stop eating so much sugar, you will get cavities”…will you though?
The belief that sugar causes cavities is another myth, one that I will dive deep into in a separate future article on dental health. Cavities are caused mostly by micronutrient deficiencies (predominantly of the fat-soluble vitamins A, D and K2), excessive bacterial proliferation in the mouth (usually due to low thyroid function which depresses immune function), and diminished saliva levels (for example, from mouth breathing).
It has been shown both in animal and human experiments that, as long as the study subjects are being fed a nutrient-dense diet, they are protected against cavities, even if their sugar intake is very high.
“In Vipeholm, Sweden, under institutionalized circumstances, patients were maintained on a variety of carbohydrate supplements to the basal, highly nutritious diet. When relatively large amounts of sucrose in solution were fed for prolonged periods of time, there was practically no increase in the incidence of dental caries.”91
One mouse study92 found that mice receiving 62% of their total calories as sucrose developed fewer cavities than mice receiving only 16% of their total calories as sucrose. The mice on the 62% sucrose diet received liver extract (which contains fat-soluble vitamins A, D and K2), B vitamins, and milk casein, which resulted in a more nutrient-dense diet high in vitamins and minerals. The other group had a nutrient-poor diet, of mostly oatmeal and dried milk, which caused them to develop cavities, even though they didn’t eat much sugar. A similar rodent study found that, when the sugar content of both diets is kept the same, only the animals on the micronutrient-deficient diet develop a lot of dental cavities.93 In short, there seems to be a strong case in support of dental cavities being caused predominantly by micronutrient deficiencies as opposed to sugar.
While studies have found that diets higher in sugar have a positive association with cavities, those diets generally tend to be lower-quality diets, missing the vitamins and minerals that protect our teeth against cavity-causing bacteria. Diets full of soda, candy, and cookies, lacking almost entirely in whole foods, are being called “high sugar diets” and the sugar is being blamed for the dental cavities - not the micronutrient deficiencies.
Additionally, the sweet foods that seem to contribute to tooth decay in studies are mostly sticky candies. By sticking to teeth, they feed mouth bacteria instead of making it down into the digestive tract where they can get fully digested and feed the person eating them. If these bacteria are pathogenic, overfeeding them can cause them to proliferate and cause dental cavities.
“When the sugar was fed in the form of sticky candies that adhered to the teeth, the incidence of dental caries increased […] In experimental animals, tooth decay does not occur unless food is present in the oral cavity […] the carbohydrate is more harmful if fed in a circumstance or in a form that will promote retention on the tooth surfaces.”94
However, again, it’s not sugar causing the cavities, but the bacteria. Keeping the metabolic rate high (which sugar helps with) can help fuel the immune system to help the body restrain these bacteria.
We Are Vilifying Sugar Instead of Focusing on the Real Problems
Here is the conclusion to all of this - no, I do not want anyone to go out and start funneling white sugar down their throat, or to start adding heaps of sugar to all their meals.
I simply believe we need to have a better understanding of what is it about many modern diets and modern foods that is so “bad.” Sugar, which is just pure energy, isn’t it. By blaming all of our problems on sugar we will never manage to solve those problems.
Coke Zero will not fix diabetes and obesity. Stevia desserts will not fix cancer. “Sugar-free” will not make us healthier. All of these approaches to nutritional policy encourage people to make the same poor dietary choices.
Instead of fighting sugar and introducing sugar taxes, how about we ensure that food deserts don’t exist? How about we teach people the basics of how our cells work and which micronutrients they need to function? How about we teach people which foods provide those micronutrients, and how to prepare them?
Sugar demonization has also contributed to some extremely silly food policies. For example, in the European Union, the Nutriscore system is placed on all packaged foods, rating them from A to E, with A being the best grade a food can receive (insinuating that it is very healthy), and E being the worst.
The other day, I purchased an organic Mango Lassi drink with only 5 simple ingredients: organic yogurt, organic mango puree, lemon juice, sugar and pectin (a fruit fibre). Want to guess the score? It was E. Simple, organic, whole-food ingredients, in a food with bioavailable calcium and protein from milk, vitamin C from lemon juice, and folate and potassium from mango. Yet, the presence of simple sucrose has garnered it the lowest possible rating.
Meanwhile, ultra-processed conventional vegan “beyond meat,” (shown above), which contains ingredients like methylcellulose (which is often derived from wood pulp processed with chloromethane and caustic soda), “flavourings,” and hexane-extracted rapeseed oil, a food that is nearly entirely micronutrient-void due to its main ingredient being improperly-prepared pea powder (peas, as other legumes, need to be soaked and thoroughly cooked to reduce lectins and other anti-nutrients), got…an A. Probably because it doesn’t have sugar.
The organic liver paté spread below also received an E rating from the European Union's “health food” rating system. Liver is one of the most nutrient-dense foods. Too bad, because in the eyes of our “experts,” the tiny bit of cane sugar added to it has entirely decimated its nutritional value.
As per this system, fresh grape juice, high in potassium, chromium, manganese, magnesium, and antioxidant polyphenols that can support a healthy microbiome, receives…you guessed it…an E.
While the cynic may say that no one should rely on a rating system for their food choices, not everyone wants to become a nutrition expert. People should be able to rely on “experts” to help them make informed decisions about their health. Such “experts” should take the time to become familiar with basic biochemistry before introducing a system that simply docks points for the presence of sugar and adds points for the presence of grains or legumes. Sadly, such due diligence hasn’t been done, and now we have ultra-processed, low-nutritional quality foods that receive an A rating, and nutritious foods that get an E simply because they have some sugar.
The food rating systems outside of the EU are no better in this aspect. The only reason why I am calling out the Nutriscore specifically is because it is the most familiar to me.
If micronutrient deficiencies as opposed to sugar are the biggest contributing factor to many (if not all) of the problems that sugar gets blamed for, then the Nutriscore (and similar systems in other countries) are harming instead of helping by dissuading consumers from buying highly nutritious foods just because they contain some sugar.
We Need to Be Looking At the Big Picture
Chronic, metabolic diseases are always multifaceted and factors that play into them include micronutrient deficiencies, poor macronutrient balance, environmental pollutants, psychosocial stress, overwork, poor light environment, developmental trauma, adverse reactions to medical interventions, latent infections, intestinal dysbiosis and so much more. Vilifying sugar will not get us anywhere closer to fixing the obesity, diabetes and chronic disease epidemic.
One might argue that all of this can be too complicated for the average person to understand, and they would be better off just avoiding sweets as it can help them unintentionally avoid junk food. However, I am of the firm belief that, as long as the information is explained simply and clearly, even someone who has no prior background in nutrition should be able to understand it. If the only information given is “sugar is bad,” then any person who decides to “cut out sugar,” yet doesn’t see any benefit, will become hopeless and feel as if they had exceeded their options. Also, if someone truly wants to better their health, simply telling them to “cut out sugar” won’t address any of the above-mentioned pillars, such as better macronutrient balance, micronutrient needs, chronic stress, etc.
Ultra-processed foods are bad because they are high in calories, low in vitamins and minerals, overuse easily oxidizable polyunsaturated fats, are often contaminated with toxic metals, contain gut-irritating additives, and use artificial flavour enhancers that promote over-eating. Sugar isn’t what makes them bad.
The quicker that we stop demonizing sugar and start addressing the real issue, which is that most people struggle with using sugar for energy due to metabolic derangements brought on by the above-mentioned factors, the closer we will get to solving the epidemic of our ever-declining health as a society.
My Substack is a reader-supported publication. If you enjoyed this article, consider becoming a paid subscriber ($15 per month or $99 for a yearly subscription), to allow me to continue devoting my time and effort to researching and writing.
Paid subscribers get full access to all of my articles and podcast episodes. My other articles dive deeper into topics such as metabolic health and fertility and dissect other health and nutrition myths.
Some of my other articles:
Content for entertainment purposes only. Not medical or health advice.
Lee JH, Duster M, Roberts T, Devinsky O. United States Dietary Trends Since 1800: Lack of Association Between Saturated Fatty Acid Consumption and Non-communicable Diseases. Front Nutr. 2022 Jan 13;8:748847. doi: 10.3389/fnut.2021.748847. PMID: 35118102; PMCID: PMC8805510.
Nerín, Cristina; Aznar, Margarita; Carrizo, Daniel . (2016). Food contamination during food process. Trends in Food Science & Technology, 48(), 63–68. doi:10.1016/j.tifs.2015.12.004
Schönfeld P, Reiser G. Why does brain metabolism not favor burning of fatty acids to provide energy? Reflections on disadvantages of the use of free fatty acids as fuel for brain. J Cereb Blood Flow Metab. 2013 Oct;33(10):1493-9. doi: 10.1038/jcbfm.2013.128. Epub 2013 Aug 7. PMID: 23921897; PMCID: PMC3790936.
Brosnan JT. Comments on metabolic needs for glucose and the role of gluconeogenesis. Eur J Clin Nutr. 1999 Apr;53 Suppl 1:S107-11. doi: 10.1038/sj.ejcn.1600748. PMID: 10365987.
Olaniyan, O.T., Dare, A., Okotie, G.E. et al. Ovarian odorant-like biomolecules in promoting chemotaxis behavior of spermatozoa olfactory receptors during migration, maturation, and fertilization. Middle East Fertil Soc J 26, 3 (2021). https://doi.org/10.1186/s43043-020-00049-w
Jinyoung Kim, Gwonhwa Song, Guoyao Wu, and Fuller W. Bazer, “Functional roles of fructose,” Texas A&M University, College Station, TX, May 23, 2012, 109 (25) E1619-E1628, https://doi.org/10.1073/pnas.1204298109
Berman, P.A.M. & Baumgarten, I. & Viljoen, D.L.. (2003). Effect of oral fructose on ethanol elimination from the bloodstream. South African Journal of Science. 99. 47-50.
Ugochukwu E. Uzuegbu; Innocent Onyesom. (2009). Fructose-induced increase in ethanol metabolism and the risk of Syndrome X in man. , 332(6), 0–538. doi:10.1016/j.crvi.2009.01.007
Ugochukwu E. Uzuegbu; Innocent Onyesom. (2009). Fructose-induced increase in ethanol metabolism and the risk of Syndrome X in man. , 332(6), 0–538. doi:10.1016/j.crvi.2009.01.007
Shafrir E. Overnutrition in spiny mice (Acomys cahirinus): beta-cell expansion leading to rupture and overt diabetes on fat-rich diet and protective energy-wasting elevation in thyroid hormone on sucrose-rich diet. Diabetes Metab Res Rev. 2000 Mar-Apr;16(2):94-105. doi: 10.1002/(sici)1520-7560(200003/04)16:2<94::aid-dmrr82>3.0.co;2-u. PMID: 10751749.
Pałkowska-Goździk E, Bigos A, Rosołowska-Huszcz D. Type of sweet flavour carrier affects thyroid axis activity in male rats. Eur J Nutr. 2018 Mar;57(2):773-782. doi: 10.1007/s00394-016-1367-x. Epub 2016 Dec 31. PMID: 28040879; PMCID: PMC5845588.
Fröhlich E, Wahl R. Physiological Role and Use of Thyroid Hormone Metabolites - Potential Utility in COVID-19 Patients. Front Endocrinol (Lausanne). 2021 Apr 26;12:587518. doi: 10.3389/fendo.2021.587518. PMID: 33981284; PMCID: PMC8109250.
Muralidhara DV, Shetty PS. Sucrose feeding stimulates basal metabolism & nonshivering thermogenesis in undernourished rats. Indian J Med Res. 1990 Dec;92:447-51. PMID: 2079362.
Sharief NN, Macdonald I. Differences in dietary-induced thermogenesis with various carbohydrates in normal and overweight men. Am J Clin Nutr. 1982 Feb;35(2):267-72. doi: 10.1093/ajcn/35.2.267. PMID: 6801959.
Hill, J O; Prentice, A M . (1995). Sugar and body weight regulation. The American Journal of Clinical Nutrition, 62(1), 264S–273S. doi:10.1093/ajcn/62.1.264S
Hill, J O; Prentice, A M . (1995). Sugar and body weight regulation. The American Journal of Clinical Nutrition, 62(1), 264S–273S. doi:10.1093/ajcn/62.1.264S
Karalis K, Goodwin G, Majzoub JA. Cortisol blockade of progesterone: a possible molecular mechanism involved in the initiation of human labor. Nat Med. 1996 May;2(5):556-60. doi: 10.1038/nm0596-556. PMID: 8616715.
Bataa M, Abdelmessih E, Hanna F. Exploring Progesterone Deficiency in First-Trimester Miscarriage and the Impact of Hormone Therapy on Foetal Development: A Scoping Review. Children (Basel). 2024 Apr 2;11(4):422. doi: 10.3390/children11040422. PMID: 38671639; PMCID: PMC11049201.
Tobiansky, D. J., Kachkovski, G. V., Enos, R. T., Schmidt, K. L., Murphy, E. A., & Soma, K. K. (2020). Sucrose consumption alters steroid and dopamine signalling in the female rat brain. Journal of Endocrinology, 245(2), 231-246. https://doi.org/10.1530/JOE-19-0386
Nätt D, Kugelberg U, Casas E, Nedstrand E, Zalavary S, Henriksson P, Nijm C, Jäderquist J, Sandborg J, Flinke E, Ramesh R, Örkenby L, Appelkvist F, Lingg T, Guzzi N, Bellodi C, Löf M, Vavouri T, Öst A. Human sperm displays rapid responses to diet. PLoS Biol. 2019 Dec 26;17(12):e3000559. doi: 10.1371/journal.pbio.3000559. PMID: 31877125; PMCID: PMC6932762.
Nätt D, Kugelberg U, Casas E, Nedstrand E, Zalavary S, Henriksson P, Nijm C, Jäderquist J, Sandborg J, Flinke E, Ramesh R, Örkenby L, Appelkvist F, Lingg T, Guzzi N, Bellodi C, Löf M, Vavouri T, Öst A. Human sperm displays rapid responses to diet. PLoS Biol. 2019 Dec 26;17(12):e3000559. doi: 10.1371/journal.pbio.3000559. PMID: 31877125; PMCID: PMC6932762.
Ulrich-Lai YM. Self-medication with sucrose. Curr Opin Behav Sci. 2016 Jun;9:78-83. doi: 10.1016/j.cobeha.2016.02.015. PMID: 26977424; PMCID: PMC4787559.
Di Polito N, Stylianakis AA, Richardson R, Baker KD. Real-World Intake of Dietary Sugars Is Associated with Reduced Cortisol Reactivity Following an Acute Physiological Stressor. Nutrients. 2023 Jan 1;15(1):209. doi: 10.3390/nu15010209. PMID: 36615866; PMCID: PMC9823716.
Dess, N. K., Choe, S., & Minor, T. R. (1998). The interaction of diet and stress in rats: High-energy food and sucrose treatment. Journal of Experimental Psychology: Animal Behavior Processes, 24(1), 60–71. https://doi.org/10.1037/0097-7403.24.1.60
Laugero, K. D.; Bell, M. E.; Bhatnagar, S.; Soriano, L.; Dallman, M. F. . (2001). Sucrose Ingestion Normalizes Central Expression of Corticotropin-Releasing-Factor Messenger Ribonucleic Acid and Energy Balance in Adrenalectomized Rats: A Glucocorticoid-Metabolic-Brain Axis?. Endocrinology, 142(7), 2796–2804. doi:10.1210/endo.142.7.8250
Balamurugan Ramadass; Karol Dokladny; Pope L. Moseley; Yatin R. Patel; Henry C. Lin. (2010). Sucrose Co-administration Reduces the Toxic Effect of Lectin on Gut Permeability and Intestinal Bacterial Colonization. , 55(10), 2778–2784. doi:10.1007/s10620-010-1359-2
Topham J. Sugar for wounds. J Tissue Viability. 2000 Jul;10(3):86-9. doi: 10.1016/s0965-206x(00)80035-2. PMID: 11299571.
Topham J. Sugar for wounds. J Tissue Viability. 2000 Jul;10(3):86-9. doi: 10.1016/s0965-206x(00)80035-2. PMID: 11299571.
Topham, J.. (2002). Why do some cavity wounds treated with honey or sugar paste heal without scarring?. Journal of Wound Care, 11(2), 53–55. doi:10.12968/jowc.2002.11.2.26372
Tan MK, Hasan Adli DS, Tumiran MA, Abdulla MA, Yusoff KM. The Efficacy of Gelam Honey Dressing towards Excisional Wound Healing. Evid Based Complement Alternat Med. 2012;2012:805932. doi: 10.1155/2012/805932. Epub 2012 Mar 28. PMID: 22536292; PMCID: PMC3320037.
Topham J. Sugar for wounds. J Tissue Viability. 2000 Jul;10(3):86-9. doi: 10.1016/s0965-206x(00)80035-2. PMID: 11299571.
Topham, j.. (1996). Sugar paste and povidone-iodine in the treatment of wounds. Journal of Wound Care, 5(8), 364–365. doi:10.12968/jowc.1996.5.8.364
Topham, J.. (2002). Why do some cavity wounds treated with honey or sugar paste heal without scarring?. Journal of Wound Care, 11(2), 53–55. doi:10.12968/jowc.2002.11.2.26
Murandu M, Webber MA, Simms MH, Dealey C. Use of granulated sugar therapy in the management of sloughy or necrotic wounds: a pilot study. J Wound Care. 2011 May;20(5):206, 208, 210 passim. doi: 10.12968/jowc.2011.20.5.206. PMID: 21647066.
Biswas A, Bharara M, Hurst C, Gruessner R, Armstrong D, Rilo H. Use of sugar on the healing of diabetic ulcers: a review. J Diabetes Sci Technol. 2010 Sep 1;4(5):1139-45. doi: 10.1177/193229681000400512. PMID: 20920433; PMCID: PMC2956799.
Shendurse, A.M.. (2016). Encyclopedia of Food and Health || Glucose: Properties and Analysis. , (), 239–247. doi:10.1016/b978-0-12-384947-2.00353-6
Sonne J, Dragsted J, Loft S, Døssing M, Andreasen F. Influence of a very low calorie diet on the clearance of oxazepam and antipyrine in man. Eur J Clin Pharmacol. 1989;36(4):407-9. doi: 10.1007/BF00558304. PMID: 2737234.
Corona-Pérez A, Díaz-Muñoz M, Rodríguez IS, Cuevas E, Martínez-Gómez M, Castelán F, Rodríguez-Antolín J, Nicolás-Toledo L. High Sucrose Intake Ameliorates the Accumulation of Hepatic Triacylglycerol Promoted by Restraint Stress in Young Rats. Lipids. 2015 Nov;50(11):1103-13. doi: 10.1007/s11745-015-4066-0. Epub 2015 Sep 23. PMID: 26399510.
Bianca Sulzbacher da Silva, Angélica Macedo Borgês Paulino, Maiara Taffarel, Ian Gabriel Borba, Luciana Ortega Telles, Victor Vitorino Lima, Danilo Henrique Aguiar, Marcos Correa Dias, André Ferreira Nascimento, Valéria Dornelles Gindri Sinhorin, Renata de Azevedo Melo Luvizotto, Gisele Facholi Bomfim, “High sucrose diet attenuates oxidative stress, inflammation and liver injury in thioacetamide-induced liver cirrhosis,” Life Sciences, Volume 267, 2021, 118944, ISSN 0024-3205, https://doi.org/10.1016/j.lfs.2020.118944.
Bianca Sulzbacher da Silva, Angélica Macedo Borgês Paulino, Maiara Taffarel, Ian Gabriel Borba, Luciana Ortega Telles, Victor Vitorino Lima, Danilo Henrique Aguiar, Marcos Correa Dias, André Ferreira Nascimento, Valéria Dornelles Gindri Sinhorin, Renata de Azevedo Melo Luvizotto, Gisele Facholi Bomfim, “High sucrose diet attenuates oxidative stress, inflammation and liver injury in thioacetamide-induced liver cirrhosis,” Life Sciences, Volume 267, 2021, 118944, ISSN 0024-3205, https://doi.org/10.1016/j.lfs.2020.118944.
Zamora Navarro S, Pérez Llamas F. Importancia de la sacarosa en las funciones coginitivas: comportamiento y conocimiento [Importance of sucrose in cognitive functions: knowledge and behavior]. Nutr Hosp. 2013 Jul;28 Suppl 4:106-11. Spanish. doi: 10.3305/nh.2013.28.sup4.6803. PMID: 23834099.
García CR, Piernas C, Martínez-Rodríguez A, Hernández-Morante JJ. Effect of glucose and sucrose on cognition in healthy humans: a systematic review and meta-analysis of interventional studies. Nutr Rev. 2021 Jan 9;79(2):171-187. doi: 10.1093/nutrit/nuaa036. PMID: 32585003.
van der Zwaluw, Nikita L.; van de Rest, Ondine; Kessels, Roy P. C.; de Groot, Lisette C. P. G. M. . (2014). Short-term effects of glucose and sucrose on cognitive performance and mood in elderly people. Journal of Clinical and Experimental Neuropsychology, 36(5), 517–527. doi:10.1080/13803395.2014.9126
Azman KF, Zakaria R. Honey as an antioxidant therapy to reduce cognitive ageing. Iran J Basic Med Sci. 2019 Dec;22(12):1368-1377. doi: 10.22038/IJBMS.2019.14027. PMID: 32133053; PMCID: PMC7043876.
Zamri NA, Ghani N, Ismail CAN, Zakaria R, Shafin N. Honey on brain health: A promising brain booster. Front Aging Neurosci. 2023 Jan 17;14:1092596. doi: 10.3389/fnagi.2022.1092596. PMID: 36733498; PMCID: PMC9887050.
MITRA A, THAKUR G. IS IQ IN NORMAL MALE STUDENTS RELATED TO THE GLUCOSE DISPOSAL RATE AND MAJOR BLOOD LIPID COMPONENTS? Journal of Clinical and Diagnostic Research [serial online] 2007 October [cited: 2007 October 1];5:347-351., https://doi.org/10.7860/JCDR/2007/.119
Kolliniati O, Ieronymaki E, Vergadi E, Tsatsanis C. Metabolic Regulation of Macrophage Activation. J Innate Immun. 2022;14(1):51-68. doi: 10.1159/000516780. Epub 2021 Jul 9. PMID: 34247159; PMCID: PMC8787535.
Christ T, Ringleb M, Haunhorst S, Fennen L, Jordan PM, Wagner H, Puta C. The acute effects of pre- and mid-exercise carbohydrate ingestion on the immunoregulatory stress hormone release in experienced endurance athletes-a systematic review. Front Sports Act Living. 2024 Jan 26;6:1264814. doi: 10.3389/fspor.2024.1264814. PMID: 38362064; PMCID: PMC10868406.
Gunzer W, Konrad M, Pail E. Exercise-induced immunodepression in endurance athletes and nutritional intervention with carbohydrate, protein and fat-what is possible, what is not? Nutrients. 2012 Sep;4(9):1187-1212. doi: 10.3390/nu4091187. Epub 2012 Sep 4. PMID: 23112908; PMCID: PMC3475230.
Murphy, E. A.; Davis, J. M.; Carmichael, M. D.; Mayer, E. P.; Ghaffar, A. . (2009). Benefits of oat -glucan and sucrose feedings on infection and macrophage antiviral resistance following exercise stress. AJP: Regulatory, Integrative and Comparative Physiology, 297(4), R1188–R1194. doi:10.1152/ajpregu.00396.2009
Murphy, E. A.; Davis, J. M.; Carmichael, M. D.; Mayer, E. P.; Ghaffar, A. . (2009). Benefits of oat -glucan and sucrose feedings on infection and macrophage antiviral resistance following exercise stress. AJP: Regulatory, Integrative and Comparative Physiology, 297(4), R1188–R1194. doi:10.1152/ajpregu.00396.2009
Borgen I, Aamodt G, Harsem N, Haugen M, Meltzer HM, Brantsæter AL. Maternal sugar consumption and risk of preeclampsia in nulliparous Norwegian women. Eur J Clin Nutr. 2012 Aug;66(8):920-5. doi: 10.1038/ejcn.2012.61. Epub 2012 Jun 20. PMID: 22713766.
Zamora Navarro S, Pérez Llamas F. Importancia de la sacarosa en las funciones coginitivas: comportamiento y conocimiento [Importance of sucrose in cognitive functions: knowledge and behavior]. Nutr Hosp. 2013 Jul;28 Suppl 4:106-11. Spanish. doi: 10.3305/nh.2013.28.sup4.6803. PMID: 23834099.
Straznicky NE, O'Callaghan CJ, Barrington VE, Louis WJ. Hypotensive effect of low-fat, high-carbohydrate diet can be independent of changes in plasma insulin concentrations. Hypertension. 1999 Oct;34(4 Pt 1):580-5. doi: 10.1161/01.hyp.34.4.580. PMID: 10523330.
Gibson S, Gunn P, Wittekind A, Cottrell R. The effects of sucrose on metabolic health: a systematic review of human intervention studies in healthy adults. Crit Rev Food Sci Nutr. 2013;53(6):591-614. doi: 10.1080/10408398.2012.691574. PMID: 23627502; PMCID: PMC3630450.
Malerbi, D. A.; Paiva, E. S. A.; Duarte, A. L.; Wajchenberg, B. L. . (1996). Metabolic Effects of Dietary Sucrose and Fructose in Type II Diabetic Subjects. Diabetes Care, 19(11), 1249–1256. doi:10.2337/diacare.19.11.1249
Kowalski, G. M.; Bruce, C. R. . (2014). The regulation of glucose metabolism: implications and considerations for the assessment of glucose homeostasis in rodents. AJP: Endocrinology and Metabolism, 307(10), E859–E871. doi:10.1152/ajpendo.00165.2014
Letexier D, Pinteur C, Large V, Fréring V, Beylot M. Comparison of the expression and activity of the lipogenic pathway in human and rat adipose tissue. J Lipid Res. 2003 Nov;44(11):2127-34. doi: 10.1194/jlr.M300235-JLR200. Epub 2003 Aug 1. PMID: 12897191.
Kaleta C, de Figueiredo LF, Werner S, Guthke R, Ristow M, Schuster S. In silico evidence for gluconeogenesis from fatty acids in humans. PLoS Comput Biol. 2011 Jul;7(7):e1002116. doi: 10.1371/journal.pcbi.1002116. Epub 2011 Jul 21. PMID: 21814506; PMCID: PMC3140964.
Zinker B, Mika A, Nguyen P, Wilcox D, Ohman L, von Geldern TW, Opgenorth T, Jacobson P. Liver-selective glucocorticoid receptor antagonism decreases glucose production and increases glucose disposal, ameliorating insulin resistance. Metabolism. 2007 Mar;56(3):380-7. doi: 10.1016/j.metabol.2006.10.021. PMID: 17292727.
Hatting M, Tavares CDJ, Sharabi K, Rines AK, Puigserver P. Insulin regulation of gluconeogenesis. Ann N Y Acad Sci. 2018 Jan;1411(1):21-35. doi: 10.1111/nyas.13435. Epub 2017 Sep 3. PMID: 28868790; PMCID: PMC5927596.
Schönfeld P, Reiser G. Why does brain metabolism not favor burning of fatty acids to provide energy? Reflections on disadvantages of the use of free fatty acids as fuel for brain. J Cereb Blood Flow Metab. 2013 Oct;33(10):1493-9. doi: 10.1038/jcbfm.2013.128. Epub 2013 Aug 7. PMID: 23921897; PMCID: PMC3790936.
Whittaker J, Harris M. Low-carbohydrate diets and men's cortisol and testosterone: Systematic review and meta-analysis. Nutr Health. 2022 Dec;28(4):543-554. doi: 10.1177/02601060221083079. Epub 2022 Mar 7. Erratum in: Nutr Health. 2022 Dec;28(4):783. doi: 10.1177/02601060221140089. PMID: 35254136; PMCID: PMC9716400.
Di Polito N, Stylianakis AA, Richardson R, Baker KD. Real-World Intake of Dietary Sugars Is Associated with Reduced Cortisol Reactivity Following an Acute Physiological Stressor. Nutrients. 2023 Jan 1;15(1):209. doi: 10.3390/nu15010209. PMID: 36615866; PMCID: PMC9823716.
Sonksen, P. (2001). Insulin, growth hormone and sport. Journal of Endocrinology, 170(1), 13-25. Retrieved Aug 9, 2024, from https://doi.org/10.1677/joe.0.1700013
Sonksen, P. (2001). Insulin, growth hormone and sport. Journal of Endocrinology, 170(1), 13-25. Retrieved Aug 9, 2024, from https://doi.org/10.1677/joe.0.1700013
BOSE JP. The role of vitamin B1 in the treatment of diabetes. Ind Med Gaz. 1949 Dec;83(12):554-6. PMID: 18117980; PMCID: PMC5200762.
Veronese N, Dominguez LJ, Pizzol D, Demurtas J, Smith L, Barbagallo M. Oral Magnesium Supplementation for Treating Glucose Metabolism Parameters in People with or at Risk of Diabetes: A Systematic Review and Meta-Analysis of Double-Blind Randomized Controlled Trials. Nutrients. 2021 Nov 15;13(11):4074. doi: 10.3390/nu13114074. PMID: 34836329; PMCID: PMC8619199.
DiPietro L, Gribok A, Stevens MS, Hamm LF, Rumpler W. Three 15-min bouts of moderate postmeal walking significantly improves 24-h glycemic control in older people at risk for impaired glucose tolerance. Diabetes Care. 2013 Oct;36(10):3262-8. doi: 10.2337/dc13-0084. Epub 2013 Jun 11. PMID: 23761134; PMCID: PMC3781561.
Navale AM, Paranjape AN. Glucose transporters: physiological and pathological roles. Biophys Rev. 2016 Mar;8(1):5-9. doi: 10.1007/s12551-015-0186-2. Epub 2016 Jan 19. PMID: 28510148; PMCID: PMC5425736.
Alan R Saltiel; Jeffrey E Pessin. (2002). Insulin signaling pathways in time and space. , 12(2), 65–71. doi:10.1016/s0962-8924(01)02207-3
Sonksen, P. (2001). Insulin, growth hormone and sport. Journal of Endocrinology, 170(1), 13-25. Retrieved Aug 9, 2024, from https://doi.org/10.1677/joe.0.1700013
Zinker B, Mika A, Nguyen P, Wilcox D, Ohman L, von Geldern TW, Opgenorth T, Jacobson P. Liver-selective glucocorticoid receptor antagonism decreases glucose production and increases glucose disposal, ameliorating insulin resistance. Metabolism. 2007 Mar;56(3):380-7. doi: 10.1016/j.metabol.2006.10.021. PMID: 17292727.
Tsatsoulis, Agathocles; Mantzaris, Michalis D.; Bellou, Sofia; Andrikoula, Maria . (2013). Insulin resistance: An adaptive mechanism becomes maladaptive in the current environment — An evolutionary perspective. Metabolism, 62(5), 622–633. doi:10.1016/j.metabol.2012.11.
Armoni M, Harel C, Bar-Yoseph F, Milo S, Karnieli E. Free fatty acids repress the GLUT4 gene expression in cardiac muscle via novel response elements. J Biol Chem. 2005 Oct 14;280(41):34786-95. doi: 10.1074/jbc.M502740200. Epub 2005 Aug 10. PMID: 16096283.
Fujisaka S, Ussar S, Clish C, Devkota S, Dreyfuss JM, Sakaguchi M, Soto M, Konishi M, Softic S, Altindis E, Li N, Gerber G, Bry L, Kahn CR. Antibiotic effects on gut microbiota and metabolism are host dependent. J Clin Invest. 2016 Dec 1;126(12):4430-4443. doi: 10.1172/JCI86674. Epub 2016 Oct 24. PMID: 27775551; PMCID: PMC5127688.
Iacovides S, Maloney SK, Bhana S, Angamia Z, Meiring RM. “Could the ketogenic diet induce a shift in thyroid function and support a metabolic advantage in healthy participants? A pilot randomized-controlled-crossover trial.” PLoS One. 2022 Jun 3;17(6):e0269440. doi: 10.1371/journal.pone.0269440.
Brosnan JT. Comments on metabolic needs for glucose and the role of gluconeogenesis. Eur J Clin Nutr. 1999 Apr;53 Suppl 1:S107-11. doi: 10.1038/sj.ejcn.1600748. PMID: 10365987.
Patel H, Kerndt CC, Bhardwaj A. Physiology, Respiratory Quotient. 2023 Feb 13. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30285389.
Fang Y, Li Z, Yang L, Li W, Wang Y, Kong Z, Miao J, Chen Y, Bian Y, Zeng L. Emerging roles of lactate in acute and chronic inflammation. Cell Commun Signal. 2024 May 16;22(1):276. doi: 10.1186/s12964-024-01624-8. PMID: 38755659; PMCID: PMC11097486.
Vander Heiden MG, Cantley LC, Thompson CB. Understanding the Warburg effect: the metabolic requirements of cell proliferation. Science. 2009 May 22;324(5930):1029-33. doi: 10.1126/science.1160809. PMID: 19460998; PMCID: PMC2849637.
Herzig, S., Shaw, R. AMPK: guardian of metabolism and mitochondrial homeostasis. Nat Rev Mol Cell Biol 19, 121–135 (2018). https://doi.org/10.1038/nrm.2017.95
Lin SC, Hardie DG. AMPK: Sensing Glucose as well as Cellular Energy Status. Cell Metab. 2018 Feb 6;27(2):299-313. doi: 10.1016/j.cmet.2017.10.009. Epub 2017 Nov 16. PMID: 29153408.
Hsu CC, Peng D, Cai Z, Lin HK. AMPK signaling and its targeting in cancer progression and treatment. Semin Cancer Biol. 2022 Oct;85:52-68. doi: 10.1016/j.semcancer.2021.04.006. Epub 2021 Apr 18. PMID: 33862221; PMCID: PMC9768867.
Crosas-Molist, E., Graziani, V., Maiques, O. et al. AMPK is a mechano-metabolic sensor linking cell adhesion and mitochondrial dynamics to Myosin-dependent cell migration. Nat Commun 14, 2740 (2023). https://doi.org/10.1038/s41467-023-38292-0
H Fraser and A T Stanton, ‘The etiology of beri-beri’, Transactions of the Society of Tropical Medicine and Hygiene, 1910, 3: 257–69, pp. 266–7.
Zamora Navarro S, Pérez Llamas F. Importancia de la sacarosa en las funciones coginitivas: comportamiento y conocimiento [Importance of sucrose in cognitive functions: knowledge and behavior]. Nutr Hosp. 2013 Jul;28 Suppl 4:106-11. Spanish. doi: 10.3305/nh.2013.28.sup4.6803. PMID: 23834099.
Bloomfield MA, McCutcheon RA, Kempton M, Freeman TP, Howes O. The effects of psychosocial stress on dopaminergic function and the acute stress response. Elife. 2019 Nov 12;8:e46797. doi: 10.7554/eLife.46797. PMID: 31711569; PMCID: PMC6850765.
Isovich E, Mijnster MJ, Flügge G, Fuchs E. Chronic psychosocial stress reduces the density of dopamine transporters. Eur J Neurosci. 2000 Mar;12(3):1071-8. doi: 10.1046/j.1460-9568.2000.00969.x. PMID: 10762338.
J. Claustre, C. Balende, J.F. Pujol, Influence of the thyroid hormone status on tyrosie hydroxylase in central and peripheral catecholaminergic structures, Neurochemistry International, Volume 28, Issue 3, 1996, Pages 277-281, ISSN 0197-0186, https://doi.org/10.1016/0197-0186(95)00088-7.
Shaw, James H.. (1958). NUTRITION AND DENTAL CARIES. Journal of the American Medical Association, 166(6), 633–. doi:10.1001/jama.1958.62990060
Constant, Marguerite A.; Phillips, Paul H.; Elvehjem, C. A. . (1952). Dental Caries in the Cotton Rat. The Journal of Nutrition, 46(3), 271–280. doi:10.1093/jn/46.3.271
Wynn, Winfrey; Haldi, John; Shaw, James H.; Sognnaes, Reidar F. . (1953). Difference in the Caries-Producing Effects of two Purified Diets Containing the Same Amount of Sugar. The Journal of Nutrition, 50(2), 267–274. doi:10.1093/jn/50.2.267
Shaw, James H.. (1958). NUTRITION AND DENTAL CARIES. Journal of the American Medical Association, 166(6), 633–. doi:10.1001/jama.1958.62990060






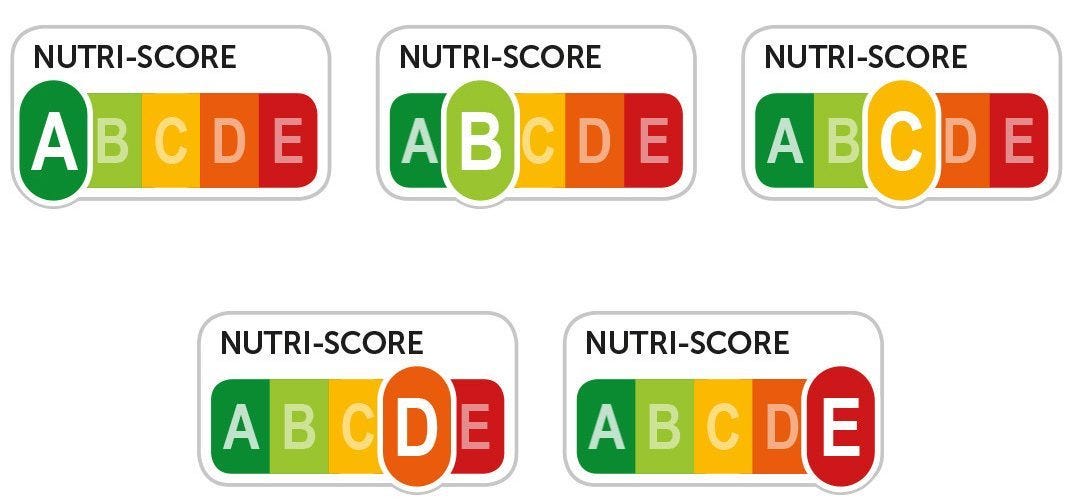






I love this!! Thank you for writing such a thorough and detailed explanation. I’m going to share with everyone I can think of. 😁
Can you please do an article (preferably with an audio recording) on weight loss for older women? Thanks.