Hypothyroidism: The Disease at the Root of All Dysfunction
Hypothyroidism often goes unnoticed because “several generations of primary care physicians and endocrinologists have been trained to treat blood tests and not patients.” - Dr. Mark Starr
Disclaimer: I am not a doctor. Content for entertainment purposes only. Not medical or health advice.
Strap in for the ride because this article goes deep. Why? Because we are here to talk about a disease that is not just a disease but THE disease. The disease at the root of all disease. Hypothyroidism. Bold statement, huh? Let’s unpack it.
But first, just before I jump into unpacking this statement, let me touch on the reason for writing this article. Although I go into this more deeply later on in the article, throughout my life I experienced multiple chronic health issues, including digestive problems, menstrual issues, recurrent infections, persistent headaches, eczema, body acne, hair loss, a tendency towards anxiety, and chronically cold hands and feet, among other things. For a very long time, I had no explanation for these symptoms, and various misguided attempts at remedying my symptoms (antibiotics, probiotics, supplements, creams, herbs, and various diets such as paleo, low-carb, dairy-free, gluten-free, sugar-free) did not yield much success.
Imagine my surprise when after connecting some dots, most of my problems spontaneously disappeared after I focused on increasing my metabolic/thyroid function, without even directly focusing on the individual problems.
Thyroid issues are often underdiagnosed and despite the plethora of doctors that I saw throughout my life, not one of them managed to link my symptoms to low metabolic function.
What I learned, and what I want to illustrate in this article, is that the body works as a single, unified system and that if something is off, it’s usually an issue with the body’s system as a whole. No organ or tissue in the body exists in isolation, and if multiple things are going wrong, there’s usually a systemic problem at play.
In this article:
Hypothyroidism: a multi-organ disorder
Diagnosis and misdiagnosis
The problems with thyroid blood tests
Unpacking thyroid blood tests
Why the TSH test is riddled with problems
The work of Dr. Broda Otto Barnes
Why having good thyroid function matters
How to self-assess thyroid function at home
Low-thyroid symptoms: a double-edged sword
High cholesterol as a sign of hypothyroidism
Low thyroid function in children
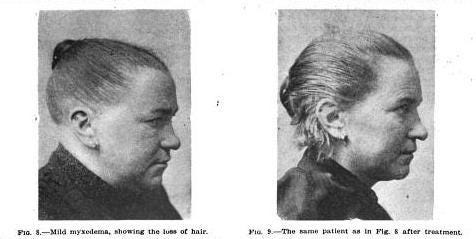
The many symptoms of hypothyroidism (with photos)
Fixing hypothyroidism
Eating in a metabolically-supportive way
Foods to prioritize
Foods to be careful with
Optimizing digestion
Food frequency & energy intake
Minimizing your toxic load
What about thyroid medication?
Conclusion
A multi-organ disorder
Traditionally, hypothyroidism is perceived as the under-activity of the thyroid gland, where the gland produces too little of the hormone T4, also known as thyroxine. However, all the symptoms of hypothyroidism can often still be experienced even if adequate T4 is made and/or administered. This is because hypothyroidism is often more complex than just the inability of the thyroid gland to produce adequate T4 and can often manifest even if the thyroid gland itself functions well. This is because hypothyroidism is a multi-organ disease, not just a disease of the thyroid gland.
Thyroxine must be converted into the active thyroid hormone, T3 (Triiodothyronine) in cells by the deiodinase enzymes1. This process takes place in multiple organs, primarily the liver, but also in the intestines, heart, kidney and other organs2, and is dependent on these organs functioning well. This conversion is also dependent on adequate selenium and iodine intake3. The activity of deiodinase enzymes can be downregulated by many factors, such as starvation, carbohydrate restriction, and heavy metals (such as mercury) that outcompete selenium.
“Starvation, and more precisely carbohydrate deprivation, appears to rapidly inhibit deiodination of T4 to T3 by type 1 iodothyronine deiodinase in the liver, thus inhibiting generation of T3.”4
“In 1952, it was recognized that T3 has greater biological potency than T4. This fundamental discovery led to the clinical concept that T4, despite being the most abundant circulating iodothyronine, functions as a prohormone, with T3 being the biologically active hormone.”5
T3 is the true thyroid hormone, while T4 is the precursor to it. T3 must then enter cells to exhibit its action, a step that takes place in every single cell in the body and that can be inhibited by stress, chemical pollutants, deficiencies, or the intake of certain foods (especially polyunsaturated oils6).
T3 in the cell is needed for the production of ATP7 (energy) from the food that we eat. ATP is the currency of the body, needed to power every single function of every single cell. The function of every organ, the production of every hormone, the repair of every tissue, and every single chemical process in the body are dependent on adequate ATP, and adequate ATP is dependent on the active thyroid hormone T3. This is why, as per the title of this article, I went ahead and made the bold claim that hypothyroidism is the disease at the root of all dysfunction, or even, the disease at the root of all disease.
A better name for hypothyroidism would be something like “low ATP disease” to divorce its association from just the thyroid gland itself.
Misunderstood and underdiagnosed
I dare to say that hypothyroidism is probably the most underdiagnosed disease in the world. One of the main reasons for this is the advent of blood tests as the “gold standard” for diagnosing hypothyroidism, with each of the tests being suboptimal (or just plain inaccurate) when it comes to actually assessing the thyroid status of an individual. In his book “Hypothyroidism Type 2: The Epidemic8,” (which goes in-depth into all the ways in which low thyroid function can manifest as various health struggles), Dr. Mark Starr sums it up perfectly when he says that “several generations of primary care physicians and endocrinologists have been trained to treat blood tests and not patients.”
I can’t count the number of people that I have interacted with who have told me about their painful periods, depression, anxiety, insomnia, fatigue, constipation, cold hands & feet, hair loss, acne, chronically dry skin and other obvious signs of thyroid dysfunction (really, even mainstream health websites like Web MD or the Mayoclinic list them as symptoms of low thyroid function), but when I suggested that if I were them I would suspect low thyroid to be the root cause, they simply correct me to tell me that it’s not possible because their blood test showed their thyroid to be “normal.” It’s sad that it took less than 50 years (because blood tests as a way of diagnosing thyroid dysfunction are a new invention) to train the general population to trust a number on a piece of paper more than their body, learning to ignore symptoms and believe that nothing is wrong because some digits on a blood test say that they are “perfectly healthy.”
I am not saying this to shame anyone as that would be the last thing that I would ever want to do. I was once one of these people, wearing a jacket inside while working my office job and still absolutely freezing, while everyone else was in a t-shirt. I was convinced that I don’t have a thyroid disorder because multiple MDs have told me that my “thyroid” is “in range.” Eventually, I learned that the term “in range” has basically no meaning. Ranges are created from the averages of the results of people visiting clinics/labs in a certain area9. And who usually goes to the doctor? Sick people. So the “range” is based on the ranges seen in sick people. And since energy (adequate ATP) must fail for disease to manifest, we can go ahead and assume that sick people are ATP-deficient, thus, hypothyroid. The ranges also differ from city to city and country to country and even lab to lab. “In range” means very little, and it can definitely mean that the person is far from the “optimal range,” even if blood tests were infallible, which they are not.
Thyroid blood tests are absurd
The title of this section might be a bit extreme, I get it. But at this point, this is kind of how I feel about most commonly used blood tests for testing thyroid function. When it comes to blood tests overall, let’s remember that blood tests show us just a quick snapshot in time. Levels of various hormones can vary greatly from hour to hour, and results can differ from lab to lab based on what the patient ate the day before, test methods, sample handling, types of equipment used, different reference values, systematic errors, etc10. Let’s also not forget that most blood tests are done in a fasted state, where a person is significantly more stressed than usual, has to run to a clinic, interact with clinic staff (which is sometimes an unpleasant experience) and then go through the anxiety of being poked with a needle. This stress itself can greatly affect blood test results. Additionally, blood tests provide a quick snapshot of what’s happening in the blood only. They give little insight into the serum concentration of different substances or whether hormones are actually getting into the cell.
Don’t get me wrong, blood tests do have their time and place when interpreted correctly such as “Why is this marker high or low” vs. the standard and reductionist form of interpretation which is “If X is high in the blood, X is high.” Blood tests have their time and place when used as one of the numerous tools to understand what is going on with the person, but never at the expense of ignoring symptoms. Sadly, nowadays a doctor can have someone sit in front of them, looking like they are an inch away from dying, and tell them that nothing is wrong because the blood test came back "in range."
Unpacking thyroid blood tests
First, let’s start with the thyroid testing “golden goose.” The one marker every doctor pays attention to. The only marker that most doctors will run to test thyroid function. The most error-prone test of all. TSH.
The TSH test was first developed pretty recently, in 1975. TSH is actually not a thyroid hormone. It is a pituitary hormone released to stimulate the thyroid to produce the thyroid prohormone T4 (thyroxine). As mentioned earlier, T4 is a pro-hormone. It is a building block - A precursor to the active form of thyroid hormone, T3 (triiodothyronine).
There are 3 big issues with TSH as a marker of thyroid health.