How to Heal MCAS and Histamine Intolerance
And why histamine issues are just the tip of the iceberg
My Substack is a reader-supported publication. To gain access to all of my articles and podcast episodes in full and to allow me to continue devoting my time and effort to my writing, consider becoming a paid subscriber ($15 per month or $99 for a yearly subscription).
The full version of this article is for paid subscribers only.
Content for entertainment purposes only. Not medical or health advice.
Questions about histamine issues and how to overcome them are some of the most common questions I receive.
While plenty of information is available on how to manage the symptoms of high histamine with “natural” compounds, clear answers as to what is causing issues with histamine intolerance or mast cell over-activation in the first place are hard to come by.
Those affected might already be familiar with low histamine diets, or herbs and supplements that help to lower histamine levels, such as nettle or DAO. However, none of these approaches get to the root of the issue, to help those afflicted with histamine issues get to a point where they can tolerate a wide array of foods, don’t have to rely chronically on antihistamines/histamine-lowering supplements, can engage in physically demanding activities without worrying about triggering an MCAS flare, and minimize the severity of (or overcome) histamine-related conditions like allergies and asthma.
High histamine levels are just the tip of the iceberg, creating some of the most unpleasant symptoms of larger, underlying problems.
If you say “I suffer from high histamine levels,” you’re not identifying the root cause behind your suffering. You’re just describing the cause of the most annoying symptoms. While high histamine levels can potentiate these larger root cause problems, they mostly signal that deeper issues need to be addressed. Without addressing these deeper layers, a person will be left simply managing symptoms of high histamine forever.
While most health blogs provide helpful recommendations to avoid high histamine foods or supplement with micronutrients that help to run the enzymes that break down histamine, they fall flat as far as helping people understand why they are dealing with this in the first place.
“Why is it that exercise gives me histamine reactions, while others are fine?”
“Why can others eat whatever they want, but I’m sensitive to nearly everything?”
“Why does my histamine intolerance flare just before my period?”
“What is histamine even, and why is it making my life miserable?”
These are some questions that most publications fail to address completely. If they do, the answer usually consists of some generic statement such as “Everyone is different, you’re just sensitive.” ✨
This doesn’t cut it for me.
Histamine is a key molecule in the body’s response to tissue damage (something that I will cover in more detail later on), and issues related to high histamine levels aren’t something that some get “cursed” with randomly because they got a bad draw in the lottery of life.
The many explanations for MCAS and its causes that I’ve seen online seem to overcomplicate the explanation, insisting that the issue is brought on by the different receptors on top of mast cells getting their wires all crossed and getting confused. I don’t think that “cellular confusion” is part of what’s happening.
Based on seeing how my histamine reactions improved simply by focusing on supporting my metabolic rate (my cells’ ability to make energy from the food I eat), and in line with the work of Dr. Ray Peat, who was a pioneering physiologist, I simply see MCAS as a body in which the threshold for inducing damage has been lowered dramatically due to the compounding effect of various environmental stressors. Even though this view might seem reductionist, it is quite cohesive when we realize that inducing tissue damage is what all the different factors that can cause mast cells to become too sensitive or to overgrow have in common.
The first half of this article will break down the contributing factors to mast cell disorders and high histamine levels, and describe the roles of histamine. The second half will focus on remediation.
In this article (table of contents):
Are Histamine Intolerance and MCAS Really So Different?
The Feedback Loops Linking Issues With Histamine Breakdown and Histamine Overproduction
The High Histamine Iceberg
Histamine Troubles and Metabolic Issues Go Hand-In-Hand
How A Low Metabolic Rate Increases Histamine Levels
A Shortage of Cellular Energy Leads to Tissue Damage and Histamine Release
“The Damage Threshold”
A Low Metabolic Rate Leads to High Estrogen and Low Progesterone Levels
A Low Metabolic Rate Slows Digestion and Can Increase Gut Histamine Levels
A Low Metabolic Rate Leads to Immune Dysfunction
Other Contributors To High Histamine Levels & Mast Cell Disorders
Dietary Deficiencies Lead To High Histamine Levels
Chronic Stress Leads to High Histamine Levels
Fasting (And Endurance Training) Can Increase Histamine Levels
PUFAs Lead to High Histamine Levels
Some Probiotics Can Cause High Histamine Levels
Environmental Estrogens and Plastics Can Increase Histamine Levels
Overtraining Can Increase Histamine Levels
Mold and Biotoxin Accumulation Can Cause Histamine Issues
Certain Drugs Can Increase Histamine Levels
Is Histamine “Evil?”
Histamine’s Many Jobs in the Body
Mast Cells Are The Body’s First Responders
Mast Cells Aren’t The Only Histamine-Producing Cells
12 Steps To Get Histamine Issues Under Control
Are Histamine Intolerance and MCAS Really So Different?
“Woah, hold on, are you covering both histamine intolerance and MCAS in one article? They’re two different things”
I am.
Many of the people I come across who suffer from high histamine levels have been researching their problem for a long time, trying to make sense of it and figure out ways to manage it. Assuming that you fall into this category, I’m sure you’ve seen claims along the lines of:
“Histamine intolerance and MCAS are very different. Don’t confuse the two!”
“MCAS is progressive and tends to get worse with time because the alterations in mast cell behaviour are permanent.”
“MCAS cannot be cured, only managed.”
I believe all of these statements to be extremely misleading, if not false, and their perpetuation is extremely demoralizing, leading those dealing with this to feel like they are broken forever. Nobody heals in a state of learned helplessness, so kicking these statements to the curb is “step 1” in getting histamine problems under control.
Histamine problems most commonly tend to be grouped into two categories: histamine intolerance and mast cell activation syndrome (MCAS).
Always emphasizing that histamine intolerance and MCAS are very different, as most resources on the topic tend to do, creates needless compartmentalization and ignores the feedback loops that closely tie the two together.
Histamine intolerance refers to the difficulty in metabolizing histamine. It is often caused by a deficiency or reduced activity of enzymes that metabolize histamine relative to the amount of histamine present in the body.
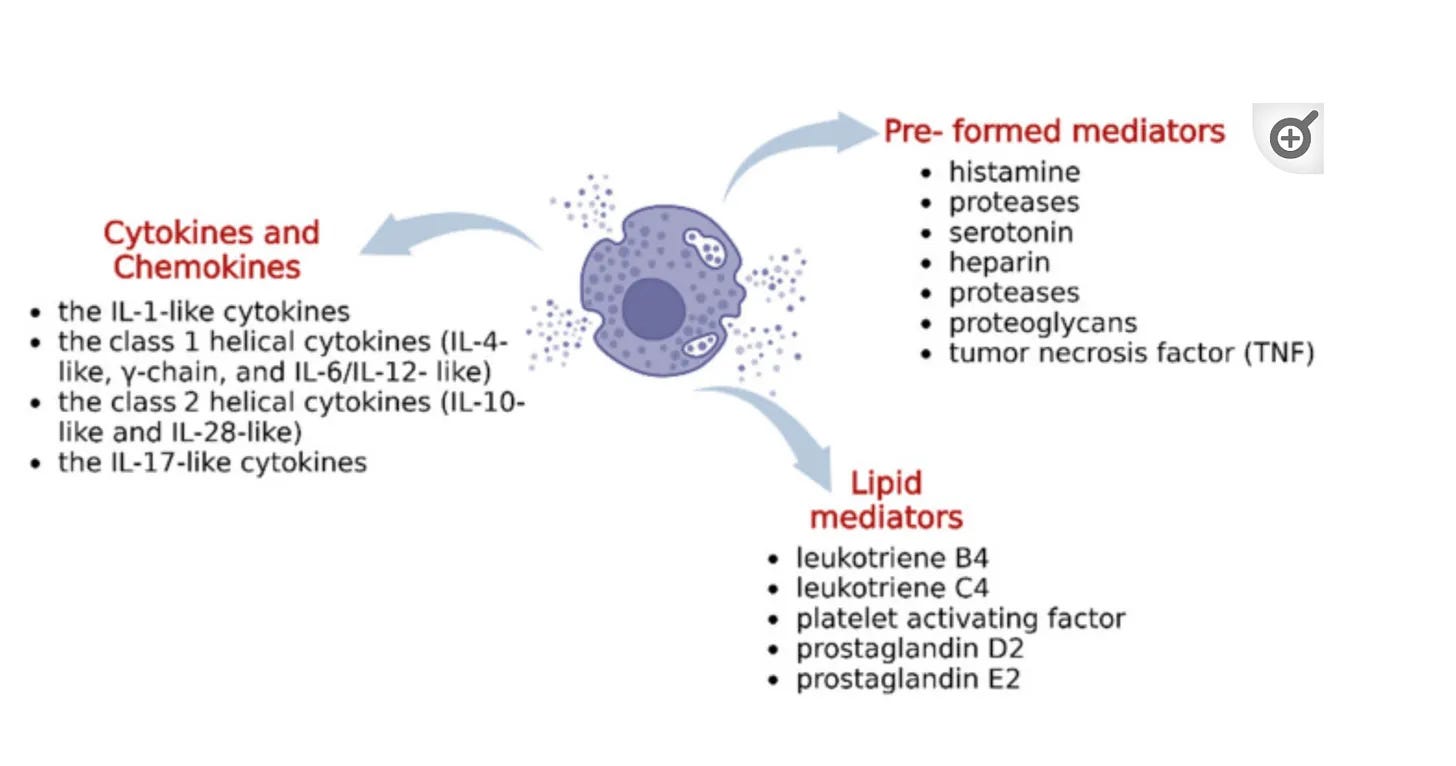
The overproduction of histamine in the body is often caused by “mast cell disorders,” such as mast cell over-activation syndrome (MCAS). Mast cells are types of immune cells that release histamine (as well as dozens of other inflammatory cytokines) in response to tissue damage or patterns associated with damage/danger. I put “mast cell disorders” in quotes because, more often than not, the overactivity or hyperplasia (overgrowth) of mast cells tends to be a response to the body’s suboptimal environment (way more on this later), so the word “disorder” rubs me a bit the wrong way. Additionally, mast cells aren’t the only cells in the body capable of producing histamine.
The Feedback Loops Linking Issues With Histamine Breakdown and Histamine Overproduction
The two main enzymes that break down histamine in the body are called DAO and HNMT.1 When the ability of DAO and HNMT to break down histamine is exceeded, as seen in histamine intolerance, histamine tends to accumulate. Histamine can cause immune cells to release inflammatory cytokines.2 These inflammatory cytokines can degranulate mast cells. Histamine can also bind to H4 histamine receptors found on mast cells, causing them to degranulate.3 In other words, histamine intolerance can drive mast cell degranulation and more histamine production.
Mast cells degranulating in the gut can add to the pool of gut histamine (from food and that produced by gut microbes) that gut enzymes have to break down, perpetuating histamine intolerance.
Histamine from the gut can enter the general circulation when the gut is leaky. Histamine itself can make the gut leaky when it accumulates (by activating H2 histamine receptors expressed in the gut).4 When the intestinal lining becomes permeable, and when the liver’s capacity to handle the escaped food particles and bacteria from the gut is exceeded, these particles can make it into the general circulation, setting off an inflammatory cascade in which mast cells are systemically degranulated.
Histamine also increases estrogen levels (both at the level of the pituitary and the ovaries),5 with estrogen being a big factor in mast cell degranulation (more on this later).
These are just a few of the feedback loops through which histamine intolerance can contribute to MCAS, and MCAS can contribute to histamine intolerance, so the two go hand in hand. Treating the two as “very different” doesn’t make senese, and can only send the person suffering from high histamine levels down the path of trying to pin point exactly which condition they have before taking action. In reality, just as improving the body’s ability to handle histamine can help with MCAS, helping to stabilize mast cells can help the body handle more histamine. Where there are feedback loops, there are multiple fronts from which the issue can be addressed.
The High Histamine Iceberg
The sentiment that leads to MCAS often being treated as something that cannot be cured but only managed stems from the fact that the causes of histamine overproduction are multifaceted and there is often more than one factor involved.
Larger, systemic issues, like estrogen dominance, hypothyroidism (low metabolic rate), infections, frequent HPA axis activation, biotoxin accumulation or PTSD, are some of the causes of histamine overproduction (and impaired histamine clearance), which will need to be addressed to get mast cells to calm down and stop releasing histamine and other inflammatory mediators.
While some blogs try to pin point the root cause of mast cell disorders and high histamine levels onto diagnostic labels such as dysautonomia, immunodeficiency, leaky gut, POTS, or autoimmunity, these are not root causes. Some of these labels simply describe a cluster of symptoms brought on by histamine, and all of them tend to be consequences of a body suffering from a shortage of cellular energy due to cumulative damage from various stressors.
You might be dealing with histamine issues without even realizing it, as the symptoms to which it contributes don’t just stop at allergies, dizziness, inability to eat cured meats and flushing, but can also manifest as painful menstrual cycles, PMDD, digestive issues, mood disorders, OCD, insomnia or motion sickness. Since histamine can increase the levels of certain neurotransmitters (such as serotonin, dopamine, acetylcholine, and noradrenaline), as well as estrogen,6 and since these are so intimately involved in controlling metabolic health, it is no wonder that histamine issues can manifest in so many varied ways, both physically and mentally.
As it happens, the iceberg flows both ways: just as the layers of it can cause histamine issues, histamine itself can potentiate the problems within each layer. Feedback loops will be a theme of this article. As you will soon find out, this is a behemoth of a topic.
By understanding histamine, how it benefits us in adequate amounts but harms in excess, what purpose(s) it serves in the body, how all the layers of the above iceberg contribute to histamine issues, and how to remediate each layer, it’s possible to make sense of the situation and start addressing it at the core.
Histamine Troubles and Metabolic Issues Go Hand-In-Hand
In my childhood and during my early 20s, my skin would often flush with redness, often without my knowing, only for me to become aware of it whenever someone asked “hey, why is your neck all red?” While this flushing was more likely to happen under the influence of emotional turmoil (such as when I was nervous about something or embarrassed), it wasn’t uncommon for me to have random red patches come and go. I didn’t think much of it at the time, nor did I make the connection that this frequent flushing could be signaling a problem.
The skin flushing was just one of my skin peculiarities. Others included eczema (which would flare in the winter or when around animals, as I’ve been allergic to pet dander most of my life) and my ability to play “tic, tac, toe” on my arm with just a few scratches.
Later in life, I started experiencing waking insomnia: I would wake up at around 3 in the morning, with racing thoughts, unable to fall back asleep. The first time this happened, it seemed to follow shortly after I took a round of probiotics on the recommendation of a chiropractor, which is something that I talked about in my gut health article. The second time I experienced this was during a time that, in retrospect, I would describe as very emotionally stressful.
Now I know that all of these skin peculiarities, insomnia, racing thoughts, chronic bloating and many of the quirks that made up my personality had one common thing underlying them: high histamine levels.
Since my histamine symptoms (apart from the insomnia) weren’t debilitating, and since they were a “normal” part of my day-to-day life, I never really registered them as an issue and never really worked to address them directly.
However, in 2019, after I started actively addressing my hypothyroidism, one of my first symptoms to disappear was my eczema, which flared only once that year (after eating some food that was at the time hard for me to digest) and not at all since. I also no longer get random red skin flushing and have lost the ability to entertain myself by playing “tic, tac, toe” by irritating my skin, as scratching no longer causes me any bumps and swelling. My sleep got better too.
How could it be that addressing my metabolic health (with practices like eating enough calories daily, hitting my micronutrient targets, cutting out polyunsaturated fats, ensuring multiple daily bowel movements, using progesterone and pregnenolone, and taking desiccated thyroid, among others) seemingly resolved my histamine issues?
Well, histamine issues and a low metabolic rate go hand in hand, and many of the cellular and hormonal derangements caused by having a low metabolic rate increase histamine levels both directly and indirectly.
How A Low Metabolic Rate Increases Histamine Levels
“A significant increase in degranulating MCs [mast cells] was observed in hypothyroid tissues, relative to euthyroid tissues. At the ultrastructural level, the MCs [mast cells] of euthyroid rats were predominantly non-degranulating (Stage I). In hypothyroid animals, numerous MCs [mast cells] showed partial degranulation (Stage II–III) or were in a stage of complete degranulation. (…) The histamine content in hypothyroid animals was higher by about 50% in the cheek skin, 25% in the exorbital lacrimal gland, and 32% in the back skin.”
- doi: 10.3390/ani12141840.
The term “low metabolism” is usually associated with being sluggish and gaining fat easily, but in reality, a low metabolism is a state in which cells lack adequate cellular energy; a state that can have many manifestations.
Cells need adequate cellular energy to maintain their function and structure and to repair damage. Even controlled cell death (apoptosis), is energy-dependent. This energy is generated from the foods we eat (carbs, protein and fats) by every cell, a process dependent on a variety of micronutrients (such as vitamins B1, B2, B7, magnesium, zinc and copper, as some examples) and adequate intracellular levels of the active thyroid hormone (T3) and oxygen. The active thyroid hormone, T3 (triiodothyronine), controls the speed at which cells generate energy from the foods we eat. The process through which cells generate energy is called cellular respiration.
When there is a shortage of any of these factors (such as thyroid hormone, oxygen, macronutrients, or specific micronutrients), or when faced with too many factors that can inhibit parts of cellular respiration (such as toxic metals, bacterial toxins, nitric oxide, carbon monoxide, or high estrogen levels), cells can struggle to generate enough energy.
A low metabolic rate makes the body less resilient to damage, causes chronic over-activation of the HPA axis, slows down detoxification pathways, interferes with the creation of protective hormones (like progesterone and pregnenolone), deprives tissues of oxygen, interferes with the body’s defences against pathogenic viruses and bacteria, and makes it harder for the body to maintain the structure of its tissues (including the gut lining). This will all be covered in more detail in the sections below.
Thyroid hormones lower the number of mast cells and lower histamine release. Anti-thyroid drugs have the opposite effect.7
A low body temperature (as seen in hypothyroidism) is a stressor in and of itself, as many of the vital enzymes in the human body function their best at a core temperature of 37°C/98.6°F, with a temperature below that reducing their function. For example, a low metabolic rate can reduce the activity of DAO and HNMT,8 the enzymes that break down histamine.
When enzymatic function is slowed, the body has a harder time maintaining itself and is more prone to damage. It was found that mast cells are a lot more likely to degranulate and release histamine at temperatures of 35°C as opposed to 37°C.9 A core body temperature two degrees lower than normal is not uncommon in hypothyroidism, and the fact that cold outdoor temperatures can drop someone’s core body temperature even lower explains in part why asthma attacks (which are driven by high histamine levels) are commonly triggered by being out in the cold.10
All the ways in which a low metabolic rate makes the body more likely to produce and release histamine,11 in both direct and indirect ways, are explained in more detail below:
A Shortage of Cellular Energy Leads to Tissue Damage and Histamine Release
“When various kinds of cells are deprived of energy (mast cells are often studied) they tend to produce (and secrete) histamine (among other substances).”
- Ray Peat, PhD, from: “Solving Some of the Problems of Aging,” Townsend Letter for Doctors, January 1991
Histamine is released in response to cell/tissue damage to bring healing factors to the damaged cells. While histamine is a molecule with diverse roles in the body (with the roles of histamine being something that I will explore later on in this article), its key role is in the immune response.
As explored in my article on Hashimoto’s disease, the immune system doesn’t just react to foreign pathogens or allergens. It responds to tissue damage and patterns that it associates with damage and danger. This is irrespective of whether this damage is caused by a pathogenic bacteria or virus, by physical trauma, pesticides, or a catabolic hormonal environment of the body.
“In addition to allergens, mast cells are also stimulated by a variety of different triggers that include bacteria, drugs, foods, fungi, heavy metals, organophosphates, viruses, and ‘danger signals’, as well as certain neuropeptides including corticotropin-releasing hormone (CRH), neurotensin (NT), and substance P (SP).”12
However, not everyone reacts with a histamine flare when exposed to any one of these stressors. Some people can sustain far more stressors than others, without experiencing a histamine reaction. What makes them more resilient?
“The Damage Threshold”
Understanding “the damage threshold” can help better explain how a low metabolic rate can contribute to histamine release.
Do you ever wonder why some people can press on their skin and nothing happens, yet for others, the pressed area immediately turns red? In the latter scenario (where the skin flushes), histamine levels clearly elevate. But why? Why can the same stimuli cause such different responses in different people? The answer: the damage threshold.
If you press a brand new rubber ball with your fingers, after you let go, the rubber bunces back to its original position, leaving no damage to the ball. However, if you take an old rubber ball, where the chemicals in the rubber have degraded over time due to heat and oxygen exposure, you might find that the ball ends up crumbling where you pressed it.
An inanimate object, like a rubber ball, cannot repair itself, so after being manufactured, it simply tends to see its structure gradually disintegrate over time. Unlike a rubber ball, the human body is in a constant state of self-maintenance to sustain its structure. The body’s ability to maintain its structure is dependent on cells being able to constantly make enough cellular energy out of the foods we eat.
If cells lose the ability to make energy, structure starts to crumble, with the most extreme example of this being seen shortly after death, when the production of cellular energy stops entirely. Shortly after an organism dies, its tissues become soft, fragile and water logged, as without cellular energy being produced, the body’s cells can’t maintain their structure (including being able to keep water inside the cell).
Death is an extreme example, as it is a state of total energy failure. However, many people walk around in a state of partial energy failure (with a wide severity spectrum), resulting in a chronic minor cellular energy deficit.
When cellular energy is chronically in short supply, the body has a harder time maintaining its structure, and much weaker stimuli (such as gently pressing the skin), can be enough to cause minor damage to the area and trigger histamine release.
In the example above, “energized” tissues are like the brand-new rubber ball, able to withstand lots of pressing and other minor assaults, without them causing any parts of their structure to crumble. “De-energized” tissues are like the old rubber ball, where the less stable the structure of the ball, the less it takes to damage it. In the extreme, a small breeze can be enough to crumble the rubber as if it were a flaky pastry.
A big part of the reason why some people are more sensitive than others to a greater variety of triggers that result in histamine release (such as certain foods, heat or psychological stress), is because the body’s energetic state (whether cells have all the cellular energy to meet their needs) dictates how resilient or non-resilient a person is to cellular damage, and whether their immune system reacts appropriately to the damage or the pattern of danger. In short, a low metabolic rate lowers the damage threshold, making the body more sensitive and susceptible to all types of damage.
Loss Of Structure Sends Out “Damage Signals” That Increase Histamine
When cells don’t have enough energy to repair themselves and maintain their structure, they can start leaking cellular parts into their surroundings, such as proteins, sugars, or even ATP (the energy molecule).
These “leaked parts” act as signals of damage that can directly increase histamine.13
Additionally, when the rate at which cellular energy is generated is slow, more reactive oxygen species are generated. In other words, a low metabolic rate leads to high oxidative stress, something that I wrote about in more detail in this article. Not only can these reactive oxygen species damage the cell, but they can also set off the alarm bells that signal for the release of histamine.
When structure fails in a state of low metabolism, histamine elevates in response.
A Low “Damage Threshold” Can Contribute To Eczema
Since cellular energy is needed to maintain the structure of cells and tissues, hypothyroidism (a state of cellular energy shortage) tends to disrupt the integrity of the skin barrier.14
“Thyroid hormone can accelerate skin barrier formation by increasing the activity of the enzyme cholesterol sulfate.”15
When the skin barrier is disrupted, the mast cells found in the skin become more sensitive, becoming more likely to create and release histamine (and other inflammatory mediators) whenever the skin is touched, rubbed against or scratched. This is why I was prone to hives and eczema after scratching when hypothyroid, but not after addressing my thyroid function.
A Low Metabolic Rate Leads to High Estrogen and Low Progesterone Levels
“Subnormal body temperature promotes estrogen secretion.”
- Ray Peat, PhD., from: “Repairing Immunodeficiencies,” Townsend Letter for Doctors, November 1989
“Estrogen turns on both the multiplication of mast cells and their tendency to release histamine and serotonin.”
- Ray Peat, PhD., from KMUD Interview, 3-18-16.
Estrogen increases histamine levels16 and progesterone lowers histamine levels.17 However, when the metabolic rate is low, estrogen tends to be high, and progesterone tends to be low.
It was found that when both women with and without allergies were tested for their reactivity to allergens and histamine on different days of the menstrual cycle, both groups reacted more strongly to the skin-prick test on days when their estrogen was highest.18
Since estrogen tends to be the highest starting from ovulation and throughout the luteal phase, as I discussed in this article, many women experience MCAS and/or histamine intolerance in the luteal phase (second half) of their cycle.
Why Does Estrogen Increase Histamine Levels?
Dr. Ray Peat described estrogen as a hormone of new beginnings. When looking at the larger pattern of how estrogen affects the body, it is mainly involved in cell division (making tissues grow bigger), and excitation (kicking off certain processes, starting something).
Estrogen “Turns On” Mast Cells By Making Them Take Up Calcium
Estrogen stimulates many different cell types to take up calcium. When cells take up calcium, this can cause them to fire off an action. For example, when muscle cells take up calcium, they contract. You can think of calcium as the trigger that sets off a reaction.
Since estrogen stimulates cells to take up calcium, a body with high estrogen levels is like a gun with a very sensitive trigger and a very heavy finger. It makes it too easy to “fire off.”
Estrogen causes mast cells to take up calcium, which causes them to release histamine.19 Estrogen makes mast cells (and basophils, and other cells that release histamine) more sensitive, and more likely to degranulate and release histamine at the slightest stimuli.20
Excessive excitation (called excitotoxicity, and characterized by excess calcium influx into cells) can kill cells, and it is often caused by very high levels of estrogen or glutamate. Cell death can then send out “danger signals” that signal immune cells to release histamine, creating a feedback loop. A milder degree of excess excitation can cause cells to get stuck in an “on” mode. For example, a muscle cramp is what happens when a muscle gets stuck “on” and fails to relax (“turn off”) and release intracellular calcium.21
Progesterone “Turns Off” Mast Cells And Helps Them Release Calcium
Progesterone works in ways that are largely opposite to that of estrogen, causing tissues to differentiate and specialize as opposed to grow, and being antiexcitatory21 (a relaxant). Progesterone can lower histamine by helping to stabilize mast cells (helps them “turn off”).22
“In the presence of progesterone, T-suppressor cell populations are increased and clonal lymphocyte proliferation is depressed. Progesterone also suppresses, in a dose-dependent fashion, IgE mediated histamine release from basophils.”23
“Besides being an antiestrogen, progesterone is a neurosteroid, an antiexcitotoxin, an inhibitory modulator. But these effects in the nervous system have their parallels in the immune system, where it modulates the actions of many cells, protecting the thymus, restraining mast cell degranulation, inhibiting the shock reaction. It is an antitoxin, stabilizing cell structure and function”
- Ray Peat, PhD, from: “Progesterone and ideas of ‘balance’ in ‘hormone replacement therapy’: The importance of inhibition,” Ray Peat’s Newsletter, March 2000
A Low Metabolic Rate Increases Estrogen, Lowers Progesterone, And Makes It Harder For Cells To Keep Calcium Out
In hypothyroidism, liver function and gut function are both slowed down. Some hypothyroid symptoms that reflect this are that hypothyroid individuals are worse at handling alcohol,2425 tend to get hypoglycemic between meals,26 and are often constipated,27 having bowel movements every few days as opposed to multiple times per day.
Hypothyroidism (low levels of the active thyroid hormone, which results in a low metabolic rate) has been shown to slow down estrogen metabolism while supplementing the active thyroid hormone, T3, speeds up estrogen metabolism.28 In other words, when the metabolic rate is low, the body has a harder time disposing of old estrogens.
A low metabolic rate is also a causative factor in making cells take up calcium. How well a cell can keep calcium out and how quickly it can release it is energy dependent. You can think of calcium as a person trying to get into a room by pushing on the door from the outside. If you’re in the room and you don’t want them to get in, you need to have enough strength to push back on the door and keep them out, and if they do get in and you want them out, you need to have enough strength to push them back out. The weaker you are, the more you will struggle and the longer it will take you to push them out of the room.
The ankle sign of hypothyroidism brilliantly illustrates this. Hypothyroid tissues relax much slower, as they fail to release calcium quickly enough (tired, de-energized cells struggle to push calcium “back out the door”). An extreme example of this is, once again, seen in death. “Rigor mortis” is a phenomenon where, as an organism dies, their muscles take up immense amounts of calcium, and get stuck in a hard, contracted state. When energy drops to 0, cells lose all the strength to keep calcium out. A low metabolic rate increases estrogen levels, and estrogen depresses thyroid function. Both are compounding factors in causing mast cells to take up calcium, making them stuck in “on” mode, releasing histamine and other inflammatory compounds.
As an additional factor, when a person is constipated (as is common in hypothyroidism), old estrogens excreted by the liver into the gut spend more time in the gut, increasing their reabsorption and recycling.
Progesterone production and release are also under metabolic control. Thyroid hormone is needed for the conversion of cholesterol to all downstream steroids, including progesterone. The release of progesterone by the corpus luteum after ovulation is also thyroid hormone dependent.29 As a result, a body in a state of low metabolism has a harder time making progesterone and getting rid of old estrogens, which can lead to an imbalance in progesterone and estrogen levels.
A Low Metabolic Rate Slows Digestion and Can Increase Gut Histamine Levels
Something that I talked about at length in my digestion article, is how intrinsically metabolic function is tied to gut function.
When the metabolic rate is low, the integrity of the gut is often compromised (“leaky gut”). This can allow a wide variety of allergens, together with gut bacteria and toxic bacterial byproducts, to reach the general circulation where they will trigger immune activation. Immune activation will increase histamine. Since DAO, the enzyme responsible for breaking down gut histamine, is created by the gut lining, when the gut lining is injured and de-energized, DAO production will be diminished.
“Cellular energy metabolism is the basis for maintaining the barrier functions. Energy depletion causes the endothelial cells lining blood vessels to become excessively permeable.* When cells' energy is depleted, water and various dissolved molecules are allowed to move into the cells, out of the cells, and through or around cells inappropriately.”
- Ray Peat, PhD., from: “Leakiness, aging, and cancer,” Ray Peat’s Newsletter, May 2005
*Endothelial cells are also found in the gut and contribute to controlling its “leakiness.”
DAO also breaks down other biogenic amines in the gut, such as cadaverine and putrescine (found in spoiled meat) or tyramine (found in many cheeses and fermented foods).30 This means that an overabundance of these other amines can contribute to “overwhelming” DAO’s capacity for breaking them down.
Cadaverine and putrescine can be increased by the overconsumption of meat relative to the intestine’s ability to absorb the broken-down amino acids (as in the case of a very high protein bodybuilding diet or the carnivore diet) and slow digestion. When the gut lining is injured or de-energized (interfering with amino acid absorption), and when constipated, the fermentation of amino acids and the creation of cadaverine and putrescine in the gut is more likely.
Additionally, when digestion is slow, the gut becomes hospitable to the growth and overgrowth of pathogenic bacteria and parasites. Not only can their presence trigger histamine release by causing damage and engaging the immune system in an attempt to flush them out, but many of these bacteria also produce histamine.31
“Histamine is formed by oxidative decarboxylation from the amino acid L-histidine with the enzyme histidine decarboxylase (HDC). (…) The species of bacteria with the highest histidine decarboxylase activity are Morganella morganii, Eschericha coli, Hafnia alvei, Proteus vulgaris, Proteus milabilis, Enterobacter aerogenes, Raoultella planticola, Raoultella ornithinolytica, Citrobacter freundii, Pseudomonas fluorescens, and Photobacterium damselae.”32
When it comes to gut histamine, it is both a product and a driver of a dysbiotic gut. Some particularly nasty bacteria can feed on histamine and use histamine for bacterial communication and to cause more damage to the host (the human they’re infecting), meaning that high histamine levels can both help bad bacteria thrive, and make them more dangerous.33 Some bad bacteria can directly signal mast cells to release histamine.34 Once again, feedback loops are a theme here, with high histamine often being both the product and the driver of dysfunction.
Histamine issues are intimately tied to gut problems, which are very closely tied to metabolic problems, and focusing on getting any gut infections or overgrowths under control is often an important step in lowering histamine levels.
A Low Metabolic Rate Leads to Immune Dysfunction
“When metabolism is increased, cells function at a higher rate of efficiency. They heal injuries quicker; old and diseased cells are replaced faster; and young, new cells are generated at an increased rate to replace worn-out ones. Even the immune system functions better. (…) Any health condition is made worse if the metabolic rate is slower than normal, because cells can’t heal and repair themselves as quickly. Increasing metabolic rate, therefore, provides an increased degree of protection from both degenerative and infectious illnesses.”
- Dr. Bruce Fife, N.D., from: “The Coconut Oil Miracle”
Back when my metabolism was in the toilet, I would get sick all. the. time. There often wasn’t a single month where I wasn’t down with the flu.
Since the immune system’s function is highly energy-dependent, a low metabolic rate invariably leads to some degree of immune dysfunction or immune incompetence. Something that I wrote about in the past was how Dr. Broda Barnes, a pioneer in helping to bring awareness to how many detrimental health conditions can be downstream of hypothyroidism, attributed the high prevalence of hypothyroidism in the modern world in part… to the invention of life-saving antibiotics. Since those who are born hypothyroid tend to have very weak immune systems, before antibiotics were invented, they would die of bacterial infections before reaching adulthood and having the chance to reproduce. With the advent of antibiotics, they were able to live long enough to reproduce, epigenetically passing their poor metabolic state onto their children, creating more hypothyroid people.
Hypothyroidism doesn’t only make the body more prone to bacterial or parasitic infections. Many viruses (such as those that cause the common cold) cannot replicate well in a body whose core temperature is 37°C/98.6°F, but can when the temperature drops by 1 or 2 whole degrees (which is what happens when the metabolic rate is low).3536
What this means is that, when the metabolic rate is low, infections are more likely to take place, and histamine release is always part of the body’s response to infections.
“Hypothyroidism has a detrimental effect on the immune system, which may predispose patients to infection. […] Hypothyroidism was associated with a higher risk of pneumonia. […] Patients with hypothyroidism who received TRT [thyroid hormone replacement therapy] had a lower risk of pneumonia than patients who did not.”37
More than that, when the metabolic rate is low, which results in the immune system failing to mount an adequate response to the infective agent, the infection can become chronic, causing chronic histamine elevations. The chronic inflammation then tends to become both a chronic source of histamine release and a chronic drain on the body’s energetic resources.
Long COVID and other chronic infections have been shown to cause MCAS.38
Using safe antibiotics or antivirals to eradicate infections could help to get histamine issues under control. Sometimes increasing the metabolic rate (for example, with the supplementation of thyroid hormones) is enough to eradicate an infection.
“Supraphysiologic doses of THs [thyroid hormones] (as in hyperthyroid states) or in vitro TH [thyroid hormone] treatment may induce TH1/TH2 modulation through an increase in TH1 responses and, thereby, could amplify host defenses against viral infections. […] A better understanding of the molecular basis of the anti-viral actions of THs [thyroid hormones] could eventually lead to a potential utilization of these hormones as anti-viral agents in clinical settings.”39
Other Contributors To High Histamine Levels & Mast Cell Disorders
A low metabolic rate basically opens the floodgates for what can go wrong with other systems in the body, as a shortage in cellular energy can manifest in many ways over time. Gut problems, hormonal imbalances, lingering infections and autoimmune disorders are the most common systemic consequences of a low metabolic rate.
Other external influences can compound onto a low metabolic rate (and further metabolic suppression), leading to mast cell disorders and high histamine levels.
Dietary Deficiencies Lead To High Histamine Levels
A deficiency of macronutrients, calories(!), and specific vitamins and minerals can lead to high histamine levels.
To make cellular energy, cells need to have enough substrate (food, calories) to make this energy out of. They can’t make it out of thin air. However, to turn sugars and fats into cellular energy, cells also need many vitamins and minerals, like the B vitamins, magnesium, zinc, copper, iron and manganese. To get rid of excess estrogen, cells additionally need vitamin E, vitamin C, molybdenum, choline, amino acids like cysteine and taurine. Apart from the nutrients mentioned, vitamin A (retinol), iodine and selenium are needed to make thyroid hormones and progesterone. Vitamin K2 is needed to support liver function, control calcium, and make androgens, like testosterone, which also work as anti-histamines.40
The enzymes that break down histamine also run on vitamins and minerals. While some people have genetic variations that affect the expression of these enzymes, the environmental strains on these enzymes (nutrient deficiencies being an example of environmental strain) are likely much bigger issues for most people.
DAO is expressed mostly in the gut and kidneys and is predominantly responsible for breaking down histamine originating from food and gut bacteria. HNMT is expressed in many tissues throughout the body and is mainly responsible for neutralizing intra-cellular (inside the cell) histamine.
The nutrients needed for proper DAO function include copper, magnesium, vitamin B6, vitamin C, and manganese.
The nutrients needed for proper HNMT function include vitamin B6, vitamin B9 and vitamin B12.
Chronic Stress Leads to High Histamine Levels
“Chronic mild stress for 3 weeks increased the number of mast cells in the brain and disturbed sleep in mice.”41
“Mast cells are critical for the development of allergic reactions, but also act as sensors of environmental and psychological stress.”42
During the COVID-19 lockdown (which lasted years in my part of the world), I started experiencing waking insomnia again (waking up at 3-4 am every night with racing thoughts and the inability to fall back asleep). This pattern of insomnia is an absolute dead giveaway of high histamine levels. The lockdown for me was characterized by chronic stress about the uncertainty of the situation, anger at the medical tyranny and ridiculous policies of the time, and a general theme of feeling like this stress and uncertainty will never end. It is no wonder then that my histamine levels went through the roof during this time since chronic stress is notoroious for causing mast cell disorders and high histamine levels.
When faced with a stressor, our adrenal glands (small glands above the kidneys) get the signal to release our main stress hormones, cortisol and adrenaline, to prepare for “fight or flight.” However, where does this signal come from?
The signal that tells our adrenals to release stress hormones starts in the brain, first with the release of a hormone called CRH, which is released by the hypothalamus. CRH tells the anterior pituitary (also in the brain) to release another hormone, called ACTH. ACTH then tells the adrenals to release cortisol. It’s sort of like a telephone line from the brain to the adrenal glands.
This telephone line works bi-directionally. Once cortisol rises, this sends a signal back to the brain telling it to lower CRH and ACTH.43
CRH causes mast cells to release histamine.44 Cortisol tells mast cells to stop releasing histamine (which is why it is used in asthma inhalers and sometimes as allergy medication).
Whenever we get stressed out, the brain hormone CRH gets released before cortisol gets released, and this CRH release causes histamine release.
When stress becomes chronic, the body can become desensitized to cortisol and fail to lower ACTH or CRH even when cortisol is (physiologically) high.45 Alternatively, as a consequence of chronic stress, the adrenal glands can become desensitized to ACTH, failing to release cortisol (or releasing too little cortisol), resulting in chronically high CRH levels, potentiating histamine release. In PTSD, for example, the body tends to be both in a chronic stress response while failing to complete this stress response, resulting in chronically high CRH46 and a reduced responsiveness to cortisol, or a depletion of adrenal cortisol reserves and an inability to produce enough cortisol. There is specifically a correlation between PTSD following sexual trauma and the inability to release enough cortisol.47 PTSD is a known risk factor for MCAS (mast cell activation syndrome) development.48
“Chronically elevated cortisol is commonly seen in depressed people, but giving a supplement of cortisol is effective in relieving depression. Both cortisol and […] ACTH […] inhibit the hypothalamic corticotropin release hormone, CRH. CRH is more directly associated with depression than cortisol is, and it by itself activates many inflammatory processes, including the release of histamine, cytokines, and nitric oxide. CRH is promoted in the hypothalamus (and in many other tissues) by inflammation, endotoxin, serotonin, interleukins, and prostaglandins, but also by the perception of unavoidable difficulties.”
- Ray Peat, PhD., from: “Endotoxin, stress, depression: Serotonin, starches, fatty acids, and antidotes,” Ray Peat’s Newsletter, May 2011
Chronic stress lowers the metabolic rate, and a low metabolic rate perpetuates the stressed state as an energy shortage is a stressor (which is also a reason why telling people to reduce stress by “doing yoga or meditating” without addressing the biological cause of their stress, the cellular energy shortage, is absolutely ridiculous).
While those with a low metabolic rate tend to have higher cortisol levels (due to its longer half life and slowed clearance in hypothyroidism),49 their bodies lose their sensitivity to cortisol.50 Their adrenals also become desensitized to ACTH, resulting in much higher ACTH levels,51 and sometimes high CRH levels too.52 ACTH also potentiates histamine release but in more of an indirect way, which is something that will be more relevant to, and discussed in, the “how PUFAs increase histamine levels” section.
Histamine release under the influence of CRH can become a positive feedback loop in generating more histamine. Histamine promotes the release of many inflammatory cytokines, many of which directly stimulate the hypothalamus to release CRH.53 As mentioned near the start, many positive feedback loops are involved in histamine issues. Additionally, the histamine release brought on by CRH contributes to “leaky gut,” which makes it easier for bacteria-derived gut histamine to enter the general circulation, and easier for gut toxins to reach the blood where they can potentiate mast cell degranulation further. Another feedback loop.
“Elevated CRH leads to increased bowel movements, intestinal permeability, and activity of the immune system in IBS patients”54
How Cortisol Can Put a Halt to Histamine Release
Stress increases histamine levels and mast cell degranulation. Yet cortisol, our main stress hormone, is used in inhalers to stop asthma and allergic attacks. How could that be?
The super-physiological doses of cortisol used in allergy/asthma treatments are often enough to finally bring down ACTH and CRH by sending a louder signal, one loud enough to get received by glucocorticoid receptors and finally lower ACTH and CRH. This breaks the positive feedback loop and brings histamine release to a halt.
This is why glucocorticoids (cortisol) are used as treatments for eczema, allergic reactions, and asthma (histamine is involved in all three of these).
However, since cortisol is a catabolic hormone (one of its main roles is tearing down tissues to increase blood sugar levels), over time it leads to tissue damage, loss of structure, more inflammation, and metabolic issues (for example, high cortisol levels lower thyroid function and make cells bad at burning carbohydrates for energy). This is why, when it comes to solving histamine issues, it’s important to address the core problems, the lower layers of the iceberg, instead of having to rely on glucocorticoids. The last section of this article will go through the steps for doing so.
Since CRH and ACTH are released whenever we are stressed (biologically or psychologically), stressors like fasting, an argument with a loved one, or any other form of distress, often cause histamine reactions. If a person is chronically stressed due to their low metabolic rate or unfavourable life circumstances or experiences, histamine issues become far more likely.
Fasting (And Endurance Training) Can Increase Histamine Levels
Histamine is produced out of the amino acid histidine. Histidine, as other amino acids, is a building block in the human body, and most tissues in the body (incluing muscles, skin and organs) contain histidine. When the body is in a catabolic (self-eating) state, such as when chronically under-eating, skipping meals (“intermittent fasting”), or during starvation (long term fasting), tissues get broken down to get turned into sugar (fuel), for the body to maintain itself. Amino acids (such as histidine) from tissue breakdown are first released into the blood before they are turned into sugar and burned for energy by cells.
Apart from the anti-metabolic effect of fasting (It can cause long term decreases in thyroid hormone levels, even after stopping the fasting. It also causes HPA axis activation), fasting can increase histamine in one very specific way - by increasing circulating histidine levels, as a result of tissue breakdown.55
As you can see in the table below, with each 3-hour increase in the length of the fast, blood histidine levels increased.

The lowering of thyroid hormone levels in fasting leads to lower CO2 production, since CO2 is produced as an end product of cellular respiration, a process that is thyroid hormone dependent. Since CO2 is needed to get oxygen into the cell, a depressed metabolism can lead to tissue hypoxia (lack of cellular oxygen). Hypoxia increases the expression of the enzyme histidine decarboxylase,56 which removes CO2 from histidine to form histamine.
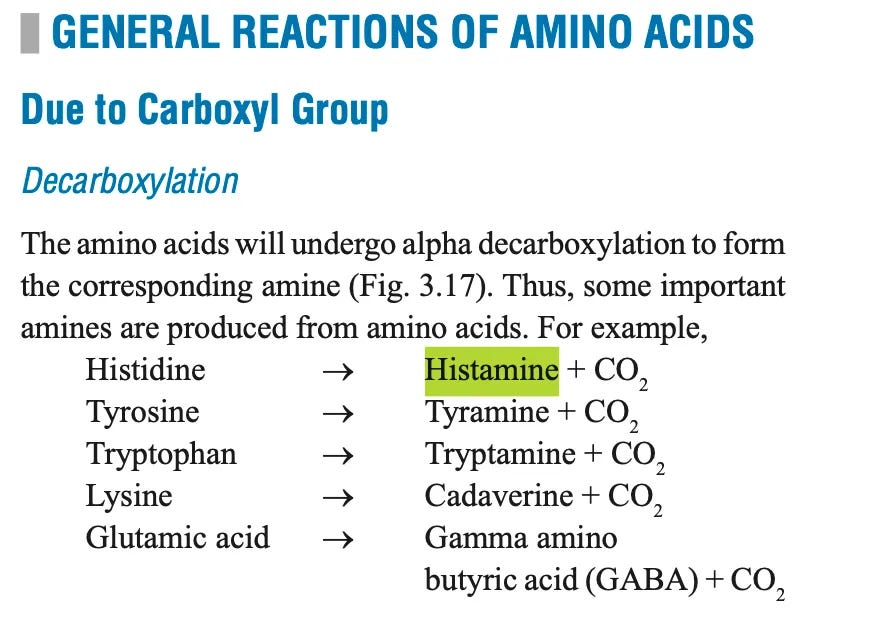
With more histidine in the general circulation, together with an environment that favours histidine decarboxylase expression, fasting, under-eating, and other practices that lead to massive tissue catabolism (such as endurance training or marathon running) can increase histamine levels. Those who have high histidine levels in the blood due to defects in histidine metabolism also present with high histamine levels, which are high not because of mast cell degranulation but as a direct product of histidine decarboxylation.57
This also applies to instances where lots of tissue damage happens due to physical trauma, releasing histidine from damaged tissues into the general circulation.
PUFAs Lead to High Histamine Levels
Since I have written at length about PUFAs (short for “polyunsaturated fats,” most commonly found in food in the form of omega-6 & omega-3 fats) in many of my articles, I won’t be going into much depth as to what they are, where they’re found, or what makes them generally dangerous in this article. For a more detailed overview on PUFAs, check out this article and this article.
Arachidonic acid is a type of omega-6 fat, found most abundantly in conventionally-farmed fatty chicken and pork, particularly when these animals are fed diets high in omega-6 fats, such as diets of corn, soybeans and canola oil. The human body can also synthesize arachidonic acid from the plant-based omega-6 fat linoleic acid found in liquid oils, such as canola oil, sunflower oil or safflower oil.
Arachidonic acid is a building block for many prostaglandins in the human body. The arachidonic acid-derived prostaglandins can be thought of as “alarm sirens” of sorts.58
Whenever there is damage in the body, these prostaglandins amplify the damage signal to recruit immune cells and repair factors to the place of damage. While this may sound like a good thing on the surface, when we have an excess of prostaglandins, the signal they release becomes too loud, and mismatched from the severity of damage. The damage signal released by a prostaglandin excess can be equated to a signal that deploys a SWAT team with an order to cut down all the trees in a forest to rescue a cat trapped in one tree. Not only is this obvious overkill, but the response creates more damage than the initial danger stimuli itself. In other words, the prostaglandin response to damage, when excessive, can create more damage. Whenever someone says that omega-6 fats are inflammatory, this is the key mechanism of action responsible for that.
Since histamine is a member of the body’s “damage response crew,” prostaglandins cause mast cells to release histamine, and the more prostaglandins in circulation, the greater the histamine release.59
ACTH (the 2nd step on our stress telephone line) causes more PUFAs to get released into the blood from fat cells and up-regulates their conversion to prostaglandins.6061 Cortisol has the opposite effect, lowering their conversion to prostaglandins.62 This is another mechanism through which chronic activation of the stress system and HPA (hypothalamus-pituitary-adrenal) axis dysfunction, leading to repeat and chronic elevations of ACTH and CRH, leads to high histamine levels and mast cell disorders.
While omega-3 fats are “anti-inflammatory” in the short term (they block the enzyme that converts omega-6 fats to prostaglandins), just like cortisol, they can cause tissue damage long term. This is because, just like omega-6 fats, they provide a substrate for free radical formation and oxidative damage. If you have no idea what any of that means (and would like to find out), check out my article: The Dark Side of Omega-3 Fats.
Some Probiotics Can Cause High Histamine Levels
As mentioned earlier, my first run in with histamine-mediated waking insomnia happened shortly after taking a round of probiotics.
As it turns out, many probiotics sold in health food shops contain bacteria capable of producing histamine. Specific probiotic bacterial strains shown to produce histamine are:63646566
Lactobacillus saerimneri 30a
Lactobacillus casei (TISTR 389)
Lactobacillus delbrueckii subsp. bulgaricus (TISTR 895)
Lactobacillus reuteri 6475
Streptococcus thermophilus CHCC1524 and CHCC6483
Anyone who struggles with histamine related issues would do best with avoiding probiotic supplements and foods that contain these bacterial strains. While there are some probiotics which help to lower histamine (which I will cover later), it is best to limit lactic acid fermented foods which do not specify the specific strain of bacteria used in the fermentation process, and to avoid probiotics which are not super transparent about the strains used. For example, if a probiotic only lists “Lactobacillus casei,” without specifying the specific strain, I would avoid it, as some strains of L. casei produce histamine and some don’t.
In my digestion article, I wrote about why I am not generally a fan of lactic acid bacteria, especially in supplemental amounts, as found in probiotics (and why I’m also not a fan of consuming large amounts of fermented foods, like sauerkraut or yogurt). Bacterial lactic acid can make it into the general circulation when the gut is leaky, and high levels of lactic acid interfere with cells’ ability to respire and make energy.67
Since many of the strains that increase histamine are from the lactobacillus family, I would probably steer clear of most supplements containing lactic acid bacteria as a general rule, as it is possible that many more of these strains create histamine too, it just hasn’t been studied yet.
Some lactic acid bacteria that can produce histamine are known to contaminate dried meats, wine or cheese,686970 which is why many with histamine issues find those foods to be triggers. For the most part, it is not the aging process itself that increases these foods’ histamine content, but the presence of bacteria. With proper food preparation methods, the growth of these bacteria becomes restrained. The same can’t be said for when a person directly introduces these bacteria into their system by taking probiotics.
Environmental Estrogens and Plastics Can Increase Histamine Levels
Estrogen is known to degranulate mast cells and is the reason why girls are more likely to develop asthma during their reproductive years71 (if they fail to produce enough progesterone to keep estrogen in check, or if their estrogen levels are very high due to environmental reasons).
Just as excess estrogen produced in the body (by the reproductive glands, adrenals and fat cells) can degranulate mast cells and cause histamine release, environmental estrogens have the same effect.72 Environmental estrogens have a compounding effect with endogenous (produced in the body) estrogens.
“Allergic diseases in childhood are closely related to environmental chemical exposure during pregnancy, including bisphenols, phthalates acid esters, perfluorochemicals, polybrominated diphenyl ethers, and polychlorinated biphenyls.”73
Some prominent environmental estrogens include the bisphenols (types of xenoestrogens found in plastic), phthalates and parabens (found in many beauty products), certain pesticides and herbicides (glyphosate, atrazine and DDT being some prominent examples, which are known for their profound toxicity yet still used in many parts of the world), metalloestrogens (toxic metals, such as nickel, cadmium and lead, which mimic the actions of estrogen in the body), brominated flame retardants (used on most furniture in certain parts of the world, including the United States. The “new car smell” is the smell of brominated flame retardants), and perfumes/fragrances.
As seen from the list above, many pesticides, toxic metals, and other pollutants can cause histamine issues, due to being estrogenic, as well as due to the fact that they can cause damage in the body, with histamine being a key responder to damage.
Since most xenoestrogens are stored in the fatty tissue of animals, it’s best to avoid fatty meat from questionable sources, where the animal may have been fed heavily sprayed foliage or given supplemental estrogens to promote growth.
You can read more about environmental estrogens and how to avoid them in my article on precocious puberty.
Plant Estrogens Can Cause Issues Too
Phytoestrogens (plant estrogens) have a similar effect. Since estrogens are intimately involved in growth, and since plants grow rapidly their entire lifecycle, it is no wonder that most plants heavily produce plant estrogens.
“Phytoestrogens are naturally-occurring plant compounds that are structurally and/or functionally similar to mammalian estrogens and their active metabolites.”74
While basically all plant foods contain phytoestrogens, most of them do not contain them in high amounts and the benefits of eating these plant foods (such as the presence of vitamins, minerals and special fibers) outweighs the phytoestrogenic concern. However, certain plant foods which are especially estrogenic are best avoided by those with histamine issues. These include flax seeds, soy, clovers, alfalfa, sesame oil, and most herbal formulas marketed as “women’s formulas,” or “menopausal formulas.”75 Some of these compounds, such as the ones derived from soy, also have a suppressive effect on the thyroid, which can slow down estrogen metabolism. Many essential oils are also estrogenic, as huge amounts of plant matter have to be condensed to create them, so it’s best not to ingest them or put them on the skin.
Traditionally-prepared soy-derived products tend to be low in phytoestrogens, but the way in which soy is being consumed in the West (in its whole form, often in the form of soybean flour or soybean oil added to processed food and used in animal feed) is highly estrogenic. The best ways to avoid soy byproducts like soybean oil and soybean flour are to avoid all types of fast food and to avoid eating at restaurants as much as possible, as most restaurants use cheap soy byproducts. Most modern vegan foods (like vegan pasta sauces or “vegan meats”) contain them too.
“Traditional Asian recipes used to prepare solid foodstuffs like Tofu, Miso, Natto, or Tempeh, empirically removed isoflavones and other soy antinutritional factors. This removal was performed by prolonged soaking and/or simmering in water. These practices allowed glycosylated isoflavones to leach into the water, which was then eliminated, taking with it most of the isoflavones. Modern Western processes, however, were designed at a time when isoflavone estrogenic effects were still being unraveled. Subsequently, to save energy and water costs, modern processing included reduced cooking durations and reduced water rinsing. Modern recipes, based on new ingredients like soy-flakes, soy-flour, or soy-juice have retained most of the isoflavones.”76
Although specific phytoestrogens (such as quercetin or resveratrol) can have a stabilizing effect on mast cells, at least in the short term, by blocking specific receptors or lowering certain inflammatory cytokines,77 long term they can add to the overall estrogenic burden of the body, worsening the problem.7879 For this reason, I am not a fan of supplementing any isolated plant flavonoids (which often come in far too high of a dose for me to consider safe) and prefer to obtain these compounds in more physiologically appropriate amounts, simply by eating fruits and vegetables in accordance with cravings.
Overtraining Can Increase Histamine Levels
“Exercise is a physical cause of allergic reactions, including exercise-induced anaphylaxis (EIAna), exercise-induced urticaria (EIU), exercise-induced asthma (EIA), and exercise-induced rhinitis (EIR).”80
Nearly 100 years ago, it was first observed that histamine levels elevate during exercise.81 This is why, for example, asthma attacks tend to be more common during or after physical activity.82 Histamine is also what contributes to sore muscles after exercise, as it makes the capillaries in the muscles more leaky to allow immune cells to enter and repair muscles.83
Apart from triggering the repair process, part of the reason for histamine release during exercise can be hyperventilation.
CO2 can prevent the degranulation of mast cells.84 It is also the body’s primary vasodilator (it dilates blood vessels to improve blood flow). When exercise becomes too intense, a person begins to hyperventilate, and when they do, they lose a lot of CO2. The loss of CO2 can cause mast cells to degranulate and release histamine. This is in part a mechanism used to release nitric oxide (the release of which is triggered by histamine), which is the body’s back-up vasodialator, used when cells are stressed for energy and when CO2 is in short supply.85
This isn’t to say that exercise is bad for health. However, what constitutes too much exercise is very person to person dependent. There is a reason why some can get an anaphylactic shock from the smallest amount of exertion while others can feel fine after an intense HIIT workout. The reason, once again, boils down to the metabolic rate.
“Hyperventilation is present in hypothyroidism, and is driven by adrenalin, lactate, and free fatty acids.”
- Ray Peat, PhD., From the article: “Altitude and Mortality”
Cells need to be able to take up oxygen to make energy. This is why the process of generating cellular energy is called cellular respiration. The reason why CO2 is so important is because tissue cells need to give red blood cells the CO2 they create to receive oxygen in return. CO2 is the currency that cells use to “buy” oxygen.
“The Haldane-Bohr effect describes the fact that oxygen and carbon dioxide destabilize each other’s binding to hemoglobin. […] Carbon dioxide, produced in the cells, releases oxygen into the tissues.”
- Ray Peat, PhD., From the article: “Altitude and Mortality”
Hypothyroidism (a low metabolic rate) creates a chronic state of hyperventilation. Hyperventilation can be thought of as a state where too much CO2 is lost or not enough produced. Since CO2 is the end product of cellular respiration, when metabolism is slow (or when in a stressed state the body has to excessively rely on burning fats for energy, which creates less CO2), too little CO2 gets produced, making it easier for the body to reach the hyperventilation threshold, even if breathing normally. It also makes it harder for cells to “purchase” the oxygen they need to make energy.
Additionally, when the body lacks the resources to adequately repair itself after a workout, the workout becomes another source of stress in an already stressed system. I recall Dr. Ray Peat mentioning in one of his interviews that in the 1800s, it was recommended for those who are hypothyroid to abstain from exercise completely during their recovery process.
The lower the metabolism is, the lower the threshold at which exercise can trigger mast cell degranulation, the greater the degree of degranulation, and the slower histamine clearance.
Thyroid hormone helps the body retain more CO2, as it inhibits the enzyme carbonic anhydrase.8687 Estrogen has the opposite effect.88
Mold and Biotoxin Accumulation Can Cause Histamine Issues
Mold exposure is often a common trigger for MCAS.89 While it is seldom an isolated cause of MCAS, it often compounds with factors like estrogen dominance, a low metabolic rate, or underlying infections.
Part of the reason why mold tends to trigger mast cell degranulation shouldn’t surprise you. Since molds, like plants, are organisms reliant on rapid growth, it should be no revelation that molds also produce their own types of growth steroids called mycoestrogens.90 “Myco” stands for mushroom, and estrogens are self-explanatory.
Main routes of mould exposure can come from hidden moulds growing in poorly ventilated and moist indoor spaces (often bathrooms or washing machines), or sometimes from the over-consumption of heavily mould-contaminated foods (such as improperly stored corn, cereals, dried fruit, coffee or peanuts).
Certain Drugs Can Increase Histamine Levels
A variety of pharmaceutical drugs (and natural compounds with similar actions) can increase histamine. These include opioids and estrogen-containing medication, such as birth control or menopausal HRT.
High doses of estrogen can inhibit the enzyme MAO-B. While normally MAO-B is used for the disposal of excess dopamine, in instances where HNMT is deficient, the body will start using MAO-B as a backup mechanism for brain histamine disposal.91 When it comes to histamine breakdown directly, high dose estrogen medication is a “double whammy,” in the sense that it can deplete the nutrients needed for HNMT function and inhibit MAO-B.
The following drugs also increase histamine levels, as they tend to inhibit DAO:92
Chloroquine
Clavulanic acid
Colistimethate
Cefuroxime
Verapamil
Clonidine
Dihydralazine
Pentamidine
Metamizole
Diclofenac
Acetylcysteine
Amitriptyline
Metoclopramide
Suxamethonium
Opioids tend to cause mast cell degranulation.93 Those who are very sensitive (or whose histamine bucket is nearly full) could also react to food-sourced opioids, such as those found in wheat or A1 casein found in dairy from some breeds of cows.94 Naltrexone (or Low Dose Naltrexone) can stabilize mast cells,95 as it is an opioid receptor blocker, which explains why those who take it often see a resolution of their insomnia, brain fog, derealization, and estrogen dominance.
Estrogen, Histamine and Serotonin: The Unholy Trinity
When mast cells degranulate, they release serotonin as well as histamine. Serotonin has been shown to increase the release of prostaglandins,9697 which can potentiate histamine release by mast cells. Another feedback loop. Serotonin has also been shown to inhibit the HNMT enzyme.98
Something that became apparent to me from Dr. Ray Peat’s writing (and from my own experiments) is that estrogen, serotonin and histamine tend to form the “unholy trinity” of inflammation. Obviously we need these compounds in adequate amounts, but bad things happen when their levels get excessive. They all tend to increase together and increase one another, while also potentiating each other’s negative effects, such as burdening the liver or slowing digestion.
By this token, many SSRIs and other serotonergic drugs can have a negative effect on histamine tolerance and increase the histaminergic burden of the body.
“A number of anti-serotonin drugs that do not block histamine much are known to exert beneficial effects on allergies and inflammatory disorders such as scleroderma, psoriasis, lupus, etc. A prime example is the class of ergot derivatives such as metergoline, lisuride, bromocriptine, and even LSD.”
- Georgi Dinkov, from the article: “Blocking serotonin may treat allergies and inflammatory diseases”
I tested the theory that lowering serotonin (without directly targeting histamine) can inhibit histamine reactions and stop the “histamine bucket” from overflowing on myself. When cleaning my closet (which triggered some sneezing since I tend to react to dust), I took Metergoline, an ergot derivative which antagonizes (blocks) many of the serotonin receptors, to see if it would stop my sneezing. Despite the fact that Metergoline is not known to target the histamine receptors at all, it stopped my sneezing and my allergic reaction.
Is Histamine “Evil?”
While you might simply associate the word histamine with that substance that makes you life miserable (especially considering just how many awful symptoms it can contribute to), the ubiquity of factors that can lead to high histamine levels should be indicative of just how vital of a compound it is.
The reason why anything that interferes with metabolism can lead to high histamine levels is because, as mentioned earlier, histamine is involved specifically in reacting to any danger and damage in the body, and the lower the metabolic rate, the lower the threshold for what’s considered damaging, explaining the greater reactivity of mast cells.
Histamine is stored in two types of cells: mast cells and basophils. However, many more cell types express the enzyme that can convert histidine to histamine, which illustrates that injury to most cell types can trigger its release, and its role is much bigger than just being involved in allergies.
Histamine’s Many Jobs in the Body
Histamine release in response to cellular damage is involved in:
Leakiness (For example, making blood vessels more leaky to allow immune cells to reach the site of tissue damage.)
Expulsion (For example, sneezing to get rid of a pollutant that reached the lungs.)
Excitation (In biology, the term excitation means “kicking something off” or “starting something.” Histamine is involved in “starts.” For example, a surge of histamine in the morning helps to wake us up. Histamine also helps to kickstart the immune response.)
When “leakiness,” “expulsion” and “excitation” happen in appropriate ways, they are helpful processes that maintain the homeostasis of the body, help us recover from damage, protect us against pollutants, and help us form new habits and memories. Unfortunately, excessive “leakiness,” “expulsion” and “excitation” become sources of disease and dysfunction in and of themselves under the influence of factors that result in an overabundance of histamine.
The next section will help you better understand histamine, as well as how “leakiness,” “expulsion,” and “excitation” can be helpful when part of an appropriate response but harmful when part of an over-exaggerated response. Since histamine is a diverse compound with diverse roles in the body, reading this next section, you might realize that some of your symptoms might be related to high histamine levels without having previously made the connection.
Leakiness
Summary of histamine’s involvement in “leakiness”
When it comes to the “leakiness” induced by histamine, when controlled, it helps to:
Get immune cells and tissue-remodeling resources to places of tissue injury to support healing.
When “leakiness” is excessive/chronic, it contributes to:
Venous insufficiency (such as varicose veins)
Edema (and associated nerve irritation)
Tissue hypoxia, leading to fibrosis
Leaky gut, bloating, peptic ulcers
Fluid build-up in the lungs
Flushing and swelling
Low blood pressure
Dizziness/vertigo
Chronic itch
Migraines
One of histamine’s main actions is making blood vessels, specifically the smallest blood vessels, the capillaries, more leaky.99 This reduces the amount of fluid in the blood as it instead allows the fluid and various particles carried in the blood (mainly the immune cells) to leak out of the blood and into tissue cells.
The vascular permeability induced by histamine is meant to allow immune cells, nutrients and proteins from the blood to enter injured tissues, where they can help to signal and facilitate their repair.
When histamine is released acutely and in appropriate amounts, its role is positive in helping to facilitate tissue repair. However, histamine’s involvement in tissue repair follows a bell shaped curve. Too little histamine and you won’t be able to deliver immune cells to the site of damage. Just the right amount, and you can repair the damage. Too much, and now the immune response itself becomes a source of damage. In de-energized tissues, leakiness can become excessive.
Under the influence of too much histamine, tissues can start retaining excessive water (edema), blood pressure can drop too low as much of the water that should be in the blood is entering tissues instead, and fluid can build up in the lungs.100 The low blood pressure caused by high histamine levels can lead to dizziness and vertigo.
The edema caused by histamine is most often seen as swelling. The complications caused by edema (excess influx of fluid, immune cells and proteins into tissues) can cause tissue damage. Under the influence of excess histamine, the inflammatory mediators, enzymes and reactive oxygen species released when too strong of an immune response is mounted can lead to tissue damage, such as tissue fibrosis. Excessive fluid uptake by tissues can irritate nerves, resulting in nerve pain, such as that seen in carpal tunnel syndrome.101
The itching caused by high histamine levels is in part caused by fluid retention, which presses onto and irritates the nerve endings of nerves near the skin. Scratching the itch usually causes more local histamine release,102 and more water (edema) to reach the scratched area, to help and “wash out” the irritant from tissues.
Histamine’s “leakiness inducing” property can also make the skin barrier more leaky, and the inflammation can impair correct tissue repair, resulting in the appearance of eczema in scratched areas.103
The increase in vascular permeability is brought on by nitric oxide, which histamine increases.104 Nitric oxide also relaxes (dilates) blood vessels and increases circulation. Nitric oxide is what can cause the redness/flushing brought on by histamine.
When nitric oxide induced venous dilation becomes chronic (as when histamine and nitric oxide are chronically high) and when veins become too dilated, failing to return to their original size, their valves fail to close properly, causing blood to pool. The pressure that the pooled blood places on the vein causes it to dilate further. This is how varicose veins, spider veins and similar venous disorders develop.105106
Since histamine also increases new vein formation,107 this too can contribute to varicose veins. Nitric oxide interferes with tissues’ ability to respire (use oxygen to make energy). Both nitric oxide and estrogen are elevated by histamine, and their hypoxic (cellular oxygen deficiency inducing) effect can cause the body to try and over-compensate by developing new veins to get oxygen to tissues.108
Since this same leakiness and tissue swelling that histamine can cause in the skin is also caused in other organs, such as the brain, histamine contributes to migraine headaches.109
Histamine’s inuction of “leakiness” isn’t contained only to blood vessels. Histamine can also cause a loosening of the tight junction proteins in the gut lining, inducing intestinal permeability, aka “leaky gut.”110 This can result in bloating, excess flatulence, and peptic ulcers.111112
Expulsion
Summary of histamine’s involvement in “expulsion”
When it comes to the “expulsion” induced by histamine, when controlled, it helps to:
Release digestive juices
Produce saliva
Expel irritants
When “expulsion” is excessive/chronic, it contributes to:
Persistent runny nose, runny eyes, or a persistent cough
Pre-term labour, miscarriage, premature ejaculation
Abdominal pains, worsening of IBS
Vomiting, motion sickness
Menstrual cramps
Diarrhea
Asthma
Nausea
Another one of histamine’s key actions is controlling the expulsion of various fluids in the body. Histamine acts as a “water-bender” of sorts. It controls many of the body’s fluids, involved both in “leakiness” and “expulsion.” In its control of “expulsion,” it stimulates the synthesis of mucus and other fluids that help to get rid of irritants, and causes contractions in various parts of the body that help to expel this irritant-containing fluid.
Histamine controls the release of gastric juices. Without histamine’s role in facilitating the release of stomach acid, we wouldn’t be able to digest protein. It also facilitates the release of saliva, which helps us sterilize the foods that enter our mouths and start starch digestion.
Histamine increases the secretion of mucus by the mucus membranes in the lungs, nose and eyes. As a result, when these membranes come in contact with an irritant, histamine helps us excrete it by making us sneeze, cough up mucus, or by making our eyes water. Histamine causes the air tubes in the lungs to constrict to make it easier for the lungs to expel mucus (kind of like squeezing a toothpaste tube to make the toothpaste come out.)
When histamine is excessive, it can lead to excessive or inappropriate expulsions.
These can include persistent sneezing, post-nasal drip, stuffy nose, watery eyes and excessive saliva production. The bronchoconstriction (narrowing of the air tubules in the lungs) which is meant to make it easier to cough up irritants can also become pathological. Excessive histamine levels can cause bronchoconstriction to become too severe, causing airways to close up, making it impossible to breathe. This is what an asthma attack looks like.113
Histamine also increases intestinal contractions to help expel toxins from the bowel. In excess, however, this can lead to abdominal pains and diarrhea.114 Histamine also increases serotonin, which pulls water into the intestines, contributing to diarrhea.
Similarly, histamine can induce “expulsion” out the other end, as it’s involved in triggering vomiting if a person ate something irritating or mildly poisonous. However, when inappropriately elevated, histamine (and the serotonin that it elevates) can contribute to persistent nausea and motion sickness.
Apart from causing the smooth muscles that make up the intestines to constrict, histamine also causes the smooth muscles of the uterus to contract. These contractions help to shed the endometrial lining (“period blood”) during menstruation. When excessive, these contractions can cause pain. Just as excessive intestinal contractions can cause “tummy aches,” the contraction of the smooth muscles of the uterus can cause menstrual pains.115
Other reproductive disturbances of “inappropriate expulsion” in which histamine is suspected to play a role are pre-term labour, miscarriage, and premature ejaculation.116117
In other words, when histamine is too high, the constriction/expulsion processes happen too aggressively, inappropriately and prematurely.
Excitation
Summary of histamine’s involvement in “excitation”
When it comes to the “excitation” induced by histamine, when controlled, it helps to:
Kick off the immune response
Control the sleep-wake cycle
Recall information
Focus
Learn
When “excitation” is excessive/chronic, it contributes to:
Tissue calcification
Racing thoughts
Arrhythmias
Insomnia
Anxiety
OCD
Histamine doesn’t just affect strictly physical functions in the body. It also affects the brain and nervous system and as a result our thoughts and personalities.
Histamine is involved in “excitation,” which is another term for “starting something” or “kicking something off.”
It kicks off the immune response when faced with cellular damage/danger.118 In the brain, histamine helps to “kick-off” the formation of new memories and thoughts. It kickstarts our ability to focus on a task.
Histamine is involved in learning and information recall, however, it can also enhance the formation of memories of painful events and lead to intrusive thoughts.119120 Histamine also increases “exploratory behaviour” and can make a person prone to always wanting to seek out novel experiences or learn about new topics.
Histamine begins to rise steadily a few hours before waking up, and an eventual rise in histamine is what wakes us up in the morning. Histamine makes us alert and ready to start the day.121
However, an excess of histamine and its excitatory action can make a person feel as if they’re “always on” without the ability to truly wind down or relax.
In a healthy nervous system and brain, a homeostasis of excitation and inhibition is needed. Think of histamine as the force needed to push yourself down a hill on a bike. Now imagine that you are rolling down the hill and want to stop. You need energy to press the brakes. If you don’t have the energy to press the brakes, you will just keep rolling. In a low energy state, where energy is lacking, a person can have an excess of “excitation” (starts), without enough energy for inhibition (bringing to a stop whatever was started).
This can present as:
Anxiety122
Insomnia123
Restlessness
Perfectionism, OCD, “type A” personality124
Waking up multiple times throughout the night
Waking up too early, and being unable to fall back asleep125
Racing thoughts (as histamine constantly “kicks off” new streams of thought)
Histamine’s excitatory action is also seen in its ability to heighten the perception of emotional pain, with high histamine levels resulting in increased emotionality and emotional sensitivity126127, while low histamine correlates with apathy. Increased emotionality could be due to histamine increasing LH, which increases estrogen levels.128
By throwing cells into “on” mode, histamine can also speed up the heart rate, which can result in arrhythmia.129 This is not to be confused with increasing the metabolism, as an excitatory state is a state of low cellular energy and energy wasting. I talk about how excitation differs from the high-energy resting state in my sleep article.
The excitatory action of histamine on nerves (turning nerves “on”) is involved both in the above-mentioned nervous system effects, as well as in the itching that histamine causes.
Histamine is also an appetite suppressant.130 A high histamine person might be high-strung, anxious, motivated, disciplined, hyper-vigilant, particular about their routine, thin (due to a suppressed appetite), emotionally sensitive/needing constant reassurance, “academically gifted” and an over-thinker.
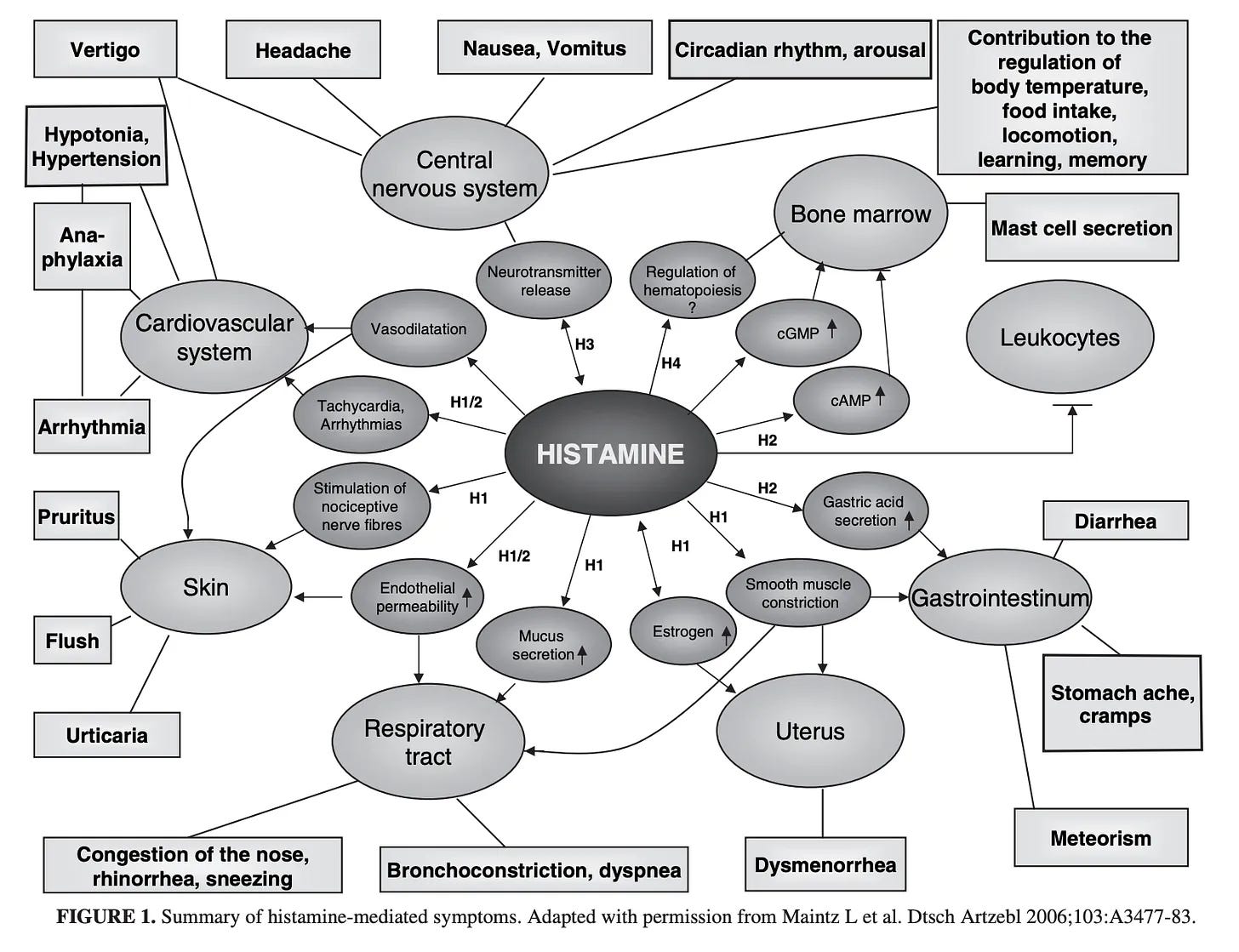
Mast Cells Are The Body’s First Responders
Mast cells are immune cells, which both create and store histamine. They are found predominantly near membranes that connect the internal environment of the body with the outside world. This includes places like the gut lining, skin, respiratory tract, blood vessels and nerves. They are the first line of defence against damage by external stimuli that our body possesses and are so vital that to this day, there has not been a single documented case of a human lacking mast cells.131 They are our body’s first line of defence from the outside world.
Histamine is produced chiefly by two types of cells in the body: mast cells and basophils.
While mast cells are best known for their role in releasing histamine, they release a whole host of other inflammatory mediators too when stimulated.132 For this reason, when a person deals with mast cells that are too sensitive (or with mast cell hyperplasia caused by factors like chronic stress), they often present with a host of other symptoms, ranging from brain fog and fatigue to autoimmune diseases, PMDD and autism, as brought on by other inflammatory mediators.133 The histamine-induced symptoms just tend to be the most distinct (such as sneezing and swelling), often alerting a person to the fact that their mast cells are actively reacting to something.
Mast Cells Aren’t The Only Histamine-Producing Cells
Basophils are the other major source of histamine produced in the body. They are a type of white blood cell. Basophils can also degranulate, releasing histamine, and just like mast cells, they too release a whole host of other inflammatory mediators.134 However, there are a few differences between the two.
While mast cells reside in tissues, basophils are short-lived and remain in the bloodstream. Basophils tend to predominantly elevate during parasitic infections (specifically worms), so a high basophil count on a blood test could be an indicator that histamine issues are brought on by parasites that the body is trying to fight.135
Eosinophils are another type of white blood cell. While they do not produce histamine, they increase predominantly in response to IgE-mediated allergens (however pollutants and chronic infections can increase them too) and can degranulate mast cells. Chronically high levels of them could potentially be a sign of an allergy to something one is exposed to often, which can result in a cross-talk between mast cells and eosinophils, where mast cells increase eosinophil recruitment to affected tissues and eosinophils degranulate mast cells and increase mast cell survival.136
Enterochromaffin-like cells (ECLs) are another histamine-releasing cell type. They are located in the stomach and stimulate histamine-mediated stomach acid release. They can overgrow and start over-producing histamine (in a sort of rebound effect) due to long-term suppression of stomach acid by factors like H.pylori infections or long-term use of proton pump inhibitor drugs.137 This can show up as developing GERD after eradicating H.pylori or discontinuing PPI drugs. H2 histamine blockers can help in this situation,138 something that will be discussed in more detail in the next section.
The enzyme that converts the amino acid histidine to histamine is expressed by a whole host of different cells in the body. Its function is up-regulated (creating more histamine) whenever these tissues are damaged by any of the multitude of factors listed in the previous section.
“The presence of HDC [histidine decarboxylase] has been reported in many human cell types, including mast cells, basophils, gastric parietal cells, and neurons. There is also evidence suggesting that this enzyme is likely present in vascular and lymphatic endothelial cells, pericytes, smooth muscle cells, and platelets.”139
How To Get Histamine Issues Under Control
You now should understand how many various stressors form feedback loops from hell to cause tissue damage and overfill the histamine bucket.
The good news is, that wherever there are many feedback loops, there are also many potential solutions, as it means that the problem can be addressed from multiple fronts all at once.
This part of the article will go through the layers of the onion, starting with the most foundational to the more granular recommendations for remediating the “iceberg” and overcoming histamine troubles. These steps should ideally be followed in order, starting with step 1, and going down the list if more support is needed, until step 12.