How to Spot Vitamin Deficiencies Based on Your Symptoms (Part 1)
A deep dive into vitamins, their functions, and how to use vitamin therapy to heal physical and psychiatric conditions
Disclaimer: This content is not intended as treatment or support for any medical condition. Content for entertainment purposes only. Not medical or health advice.
When it comes to spotting vitamin deficiencies, I believe symptoms can sometimes tell us more than tests, sometimes serving as the most useful clues.
Blood tests are commonly used to check the levels of vitamins in the blood directly, but this has significant limitations.
Blood is a “highway” that the body uses to deliver nutrients to cells. It shows which nutrients are “in transit” at a specific point in time, not how well they’re being used or stored. Often, what is observed is more of a snapshot of which nutrients are circulating after a recent meal, rather than a reflection of overall nutrient status. The body likes to keep blood micronutrient levels relatively stable, to ensure adequate delivery of life-sustaining nutrients to tissues, so systemic deficiencies might not always reveal themselves.
Certain blood markers, however, ones which don’t directly test vitamin levels, can often be more useful in spotting systemic deficiencies. These useful proxy markers instead often show which vitamin-dependent systems in the body are suffering as a result of vitamin deprivation. Rather than testing vitamin levels directly, they check for things in the body that aren’t working correctly. (This article covers these proxy markers and how to interpret them.)
Even Advanced Vitamin Tests Have Some Downsides
There are some more advanced tests available which aim to assess nutrient use and storage with increased accuracy. These include the Organic Acids Test (OAT) and SpectraCell analysis, a fairly new option.
Unfortunately, they are often very costly, and even if you can afford them, access to them can be an issue. Most conventional doctors won’t order them, as they’re not trained to interpret the results. You’d need to seek out a functional, integrative or naturopathic practitioner.
Even then, these expensive tests have their faults.
The OAT measures the metabolic byproducts (or the “footprints”) of nutrients in urine, but results can be influenced by factors outside of nutrient status, like kidney function, liver function or dehydration.
In the SpectraCell analysis, your white blood cells are collected and then shipped to a lab where they will be grown in “test tubes,” each deficient in one specific nutrient. The idea is that “well-nourished” white blood cells will be “saturated” enough with nutrients to withstand the nutrient-deficient lab environment. If their function is inhibited in any given nutrient-poor environment, the test assumes that a pre-existing functional deficiency of that specific vitamin or mineral is present.
In other words, the test sees how cells respond to missing nutrients, rather than trying to measure the body's stores of a nutrient. While the concept behind the test is interesting, it can take weeks to get results, and the jury is still out as to whether the test is even an accurate representation of nutrient status.
Test, Don’t Guess…But Don’t Blindly Trust the Tests Either
To be clear, I’m not saying you shouldn’t explore these tests. In the hands of a competent physician, they offer valuable insights.
But, together with their shortcomings, these tests might not always capture individual-specific risk factors, such as:
Genetic mutations, toxic load problems, or disease states that increase the need for the vitamin or make it less functional in the body.
Someone’s ability to absorb or utilize the vitamin.
Other underlying deficiencies that might make a vitamin non-functional, even if its levels in the body appear normal or high.
General individual-specific oddities that make it so someone needs far more than the established vitamin RDA to function normally.
The good news is that, with a bit of self-examination, there are ways to spot specific deficiencies all by yourself. This article series provides you with the tools to answer questions like:
Do I fit the picture of having multiple physical or psychological symptoms specific to the deficiency of a certain vitamin? If I treat the symptom list like a Bingo card, do most of them apply to me?
Do my general lifestyle habits fit the list of habits that put someone at risk of a specific deficiency?
Does my diet make me prone to that deficiency based on what I do (or do not) eat? *
Do my past blood tests show that certain bodily vitamin-dependent functions are operating sub-optimally, even if no direct vitamin measurements were flagged as “below range”?
*The richest food sources of a certain vitamin will be marked with a “⭐️” throughout this article.
My goal is to help my readers become more self-sufficient in managing their health. While I jokingly call the practice of relying on symptoms, cravings, and basic logic to spot deficiencies “the caveman method,” I believe that it’s anything but primitive. If anything, it’s intuitive.
After all, even if our test results show that a nutrient is “within range,” many factors can interfere with the use of nutrients, accelerate their breakdown and depletion, or make someone’s need for it higher than that of an average person. If my body is showing me deficiency symptoms, I will get curious, regardless of the test result.
Taking a good, hard look at what the body is trying to tell us can be just as (if not more) valuable than comprehensive testing. The “hack” is knowing how to understand the body’s language.
“Why Should I Even Care if I’m Vitamin Deficient?”
Despite the fact that we literally cannot survive without vitamins (the word "vital" is in the name for a reason), most people today associate the word "vitamins" with ineffective placebo do-nothing pills.
It appears to me that in the mind of the “average Joe,” the term “vitamins” has become synonymous with multi-level marketing schemes, poor-quality supplements, juice cleanses, snake oil salesmen and celebrity "skin gummies." This misalignment in perception obscures the fundamental truth that vitamins are nearly on par with oxygen when it comes to their necessity to both optimal function and basic survival.
While we often believe that modern diseases are far more complicated and sophisticated than being the manifestations of subclinical vitamin and mineral deficiencies, this is not always true. With the “branding crisis” that vitamins are currently experiencing, people rarely consider that their depression, ADHD, diabetes, autoimmunity, chronic diarrhea, hair loss, or PMS might stem from a subclinical vitamin or mineral deficiency (or multiple deficiencies). These symptoms then get treated with medications that may or may not resolve some symptoms, while failing to correct the underlying issue.
This is not just theoretical. High-dose vitamin therapy (and mineral therapy, but this I’ll cover another time) has been used to resolve conditions like schizophrenia, arthritis, bipolar disorder, cataracts, type II diabetes, and a whole other array of chronic physical and mental ailments.
The idea that a debilitating condition might just be a manifestation of a vitamin deficiency or a vitamin dependency (requiring a supra-physiological dose of a certain vitamin to resolve) is not just a meme. It’s a well-documented phenomenon.
In This Article:
This is the first part of a series diving deep into vitamins, their functions, and how their deficiencies manifest. This article covers the first four vitamins: vitamin A, vitamin B1, vitamin B2 and vitamin B3. A general intro to the topic of vitamins is also covered in this installment of the series.
The topics covered in this installment can be of particular interest to those afflicted with: arthritis, chronic fatigue syndrome, POTS, memory problems, ADHD/autism, skin conditions, cognitive decline, psychiatric disorders (schizophrenia, bipolar and unipolar depression), eye problems (glaucoma, cataracts, vision loss), diabetes, metabolic syndrome, digestive issues (gastroparesis, chronic diarrhea, SIBO, ulcerative colitis), hormonal imbalances & multiple sclerosis.
Table of Contents:
My Substack is a reader-supported publication. To gain access to all of my articles and podcast episodes in full and to allow me to continue devoting my time and effort to my writing, consider becoming a paid subscriber ($15 per month, cancel any time, or $100 for a yearly subscription).
The full version of this article is for paid subscribers only.
What Even Are Vitamins?
Vitamins were first discovered almost 140 years ago by observing what happens when a certain population lacks them. For example, when people or animals are fed diets consisting mostly of highly refined foods (like polished white rice, which we now know lacks vitamins), their health starts to fall apart. They develop deformities. Their mental health spirals, and their cognition deteriorates. Their hair falls out, their skin degenerates, their digestive system starts malfunctioning, their bones start dissolving, their heart and other organs start failing, their limbs start collapsing, and eventually, they die.
The first widely documented case recognizing that living beings require "specific unidentified food compounds" to prevent disease came from Dutch physician Christiaan Eijkman in 1889. At the time, a mysterious disease called beriberi, which we now understand as severe vitamin B1 deficiency, was devastating parts of Asia, where white rice served as the primary food staple. The disease caused muscle wasting, nerve damage, leg paralysis, and ultimately cardiovascular failure and death.
Eijikman was sent to the Dutch East Indies (present-day Indonesia) to investigate the illness. The leading theories at the time assumed beriberi to be caused by a microbe or toxin. To test these theories, Ejikman used chickens in his experiments. Oddly enough, all of his chickens, those exposed to various microbes, and the isolated, “untouched” control group, began to show symptoms of a beriberi-like illness. Then, just as inexplicably, they started recovering. Ejikman was puzzled.
Stumped for an explanation, Eijkman asked his chicken coup caretaker if anything had changed in how the chickens are being cared for. The man said that, yes, he had recently switched the birds’ diet from leftover polished white rice (from the military hospital kitchen) to cheap, feed-grade brown rice, because the cook who previously supplied the white rice decided that he would no longer “give military rice to civilian chickens!”1
Ejikman realized that brown rice must contain some sort of a “beriberi antidote compound.” This compound turned out to be vitamin B1 - a vitamin found in rice hulls but missing entirely in polished white rice.23
In a sense, one cook’s stubbornness eventually led us to the realization that food contains some peculiar and then-unidentified compounds that didn’t fit into the known categories of carbs, fats, or proteins, but which, in tiny amounts, are necessary to maintaining life. These “mysterious compounds” became known as vitamins.
Vitamins Get Their Name
Building on Ejikman’s work some two decades later, Polish biochemist Casimir (Kazimierz) Funk became the first to isolate this “anti-beriberi” factor, vitamin B1, from rice hulls. This was one of the milestones that established his legacy as “the father of vitamin therapy.” Funk was the first to popularize the revolutionary for its time concept that many diseases once attributed to microbes (like beriberi, pellagra, rickets or scurvy) were caused by a deficiency of these “mysterious but indispensable food compounds.”
In 1911, Funk named these “mysterious compounds” “vital amines,”4 drawing the "amine" portion from the amine group found in vitamin B1 (☝️🤓 amines are nitrogen-containing organic compounds that serve as precursors to proteins). He later shortened this to “vitamines,” with the prefix “vita” meaning life in Latin.
As scientists discovered more vitamins, they realized not all contained amine groups, but the name had already stuck, so we’ve just gone along with it for over a century.5 Funk himself suspected not all vitamins would contain amines, but he felt "vitamines" was catchy and memorable.6 He was right, it seems. We did drop the “e” along the way, though, with “vitamines” becoming “vitamins.”
As research progressed, we’ve discovered that vitamins are crucial for virtually every bodily function: turning foods into energy, producing neurotransmitters and staying sane, creating sex hormones and reproducing, growing tissues, maintaining organ function, preserving our skin, hair, bones and teeth, and any other bodily function you could think of.
The Essential Thirteen
We've now identified 13 essential vitamins that must be obtained through diet because the human body cannot synthesize them: vitamins A, B1, B2, B3, B5, B6, B7, B9, B12, C, D, E, and K.
Other compounds sometimes called "vitamins," like B4 (choline), B8 (inositol), and B10 (PABA), aren’t technically vitamins since they can be synthesized in the body. However, even though they don’t fully fit the vitamin classification, these compounds still have health benefits, and certain conditions improve when their dietary levels increase, especially since the amounts made in the body aren’t always sufficient.
Another “wildcard” is pyrroloquinoline quinone (PQQ), a bacteria-produced compound found in many plant foods, especially parsley and papaya.7 Discovered in 1979, PQQ is currently classified as a “vitamin-like compound” (a sort of vitamin) because while its deficiency isn’t immediately life-threatening, it does lead to worse health outcomes.
Vitamin Deficiencies Are a Silent Epidemic
Vitamin deficiencies represent a silent epidemic, even in wealthy, "over-fed" countries.
Both dietary surveys and results from measuring vitamin levels across population samples reveal that deficiency rates in many developed nations range from 50% for some vitamins to an astounding 95% for others.8910
In developing nations, the issue is far worse, with vitamin deficiencies still being the leading cause of death in some regions.
“Globally, more than two billion people are suffering from micronutrient insufficiency, especially iodine, iron, folate, vitamin A, and zinc. It is the main cause of premature deaths, morbidity, and retardation in the physical and mental growth of children; in 2017, 11 million deaths and 255 million daily-adjusted life years (DALYs) could be attributed to malnutrition.”11
Several factors compound this crisis. Chronic stress, the increasing pollution that we are exposed to, endemic gut and thyroid dysfunction, and certain genetic variations that we are still learning about, can make it so a person needs far more than the accepted vitamin RDA (recommended daily allowance) to prevent and overcome a deficiency and the associated disease states. Yet, many aren’t even meeting these theoretical RDAs!
Additionally, studies are showing that unsustainable farming practices have resulted in many crops having lower vitamin and mineral levels than they did 50 or more years ago.1213
Milder deficiencies may not be severe enough to produce the dramatic symptoms of diseases like pellagra (severe vitamin B3 deficiency causing skin to peel off) or beriberi, but they can generate a wide array of chronic health problems. Scientifically, we are not as well-versed in these milder deficiency manifestations as we are in severe deficiency diseases.
Vitamin Research Has Been Largely Sidelined
The vitamin deficiency problem is likely amplified by the fact that, in the last few decades, vitamin research has taken a back seat, with most research funding being prioritized for other areas of study.14
Once the diseases of severe vitamin deficiency were discovered and treated, the investigation into the manifestations of subtler forms of vitamin inadequacies in the body was largely overlooked.
Yet, I suspect that we might still be scratching the surface when it comes to understanding vitamins and vitamin therapy. I mean, think about it! A bit over a century ago, we didn’t know any vitamins. All of the vitamins that we know today were discovered between 1910 and 1948.
After the 1950s, scientific interest in vitamin therapies declined in popularity. Research efforts shifted to other areas, including pharmaceutical drugs, particularly after observing that drugs often create more immediate improvements in acute, life-threatening situations.
However, nowadays, we face an epidemic of chronic health conditions, not acute medical crises. Since vitamin research has been sidelined, could it be possible that there are still vitamins that we haven’t discovered yet? How many chronic health conditions could be improved by them?
More recently, some of the funding enthusiasm for vitamin research was lost after trials and surveys on the use of various vitamin supplements produced mixed results. This further muddied the distinction between vitamins and “cheap supplements” in the minds of many.
Ideology Over Biology: Fad Diets Compounding the Deficiency Epidemic
Due to better food and medical care availability, we don’t see the horror-movie-esque manifestations of severe vitamin deficiencies, ones that leave those affected looking like characters from a David Lynch movie, as often as we would a few centuries ago.
However, with the popularization of ideologically driven extreme diets (like keto, veganism, or raw foodism), we are backtracking on our progress and seeing a resurgence of diseases of severe malnutrition in wealthy societies in the West.
In countries where a few pieces of fruit, a carton of dairy milk, a couple of eggs, some green vegetables, and a few slices of meat (aka, foods that meet many if not most of our daily nutritional needs) are affordable, people are giving themselves various types and degrees of avitaminosis by eating a severely restricted set of foods, based on bad ideas and false information.
Those who are not “health obsessed” end up in the same boat, not because of orthorexic tendencies, but because eating deep-fried takeout and drinking fountain drinks isn’t providing much in the way of vitamins. There’s even a term for this: high-calorie malnutrition.
Understanding the broad spectrum of symptoms that various deficiencies can cause is crucial, as is knowing which foods provide these vitamins. Recognizing and correcting nutritional gaps could save years of confusion, preventing people from endlessly searching for the right medication to fix what might be a potential vitamin deficiency issue.
Vitamin A (Retinol)
The maintainer of mucus membranes, eyesight, beauty, growth, fertility and “robustness.”
Predominant deficiency symptoms:
blindness (including night blindness), acne, dry skin, bumpy skin (keratosis pilaris), dry eyes, cracked lips, low levels of “youth- associated” sex hormones (testosterone, progesterone, pregnenolone), infertility (male and female), frequent infections, “leaky gut,” cavities, poor bone growth, hair loss
The Importance of Retinol:
At the start of the 20th century, a time when vitamins were just being discovered, it was observed that milk contained some substance “necessary to maintaining life.”
In 1912, researchers found that rats placed on a diet of starch, protein, lard, minerals and cane sugar failed to grow and develop properly. Adding milk to their diet reversed this affliction, restoring proper growth and development. The “magical” milk substance that aided proper development, prevented eye lesions and stopped animals from wasting away and dying turned out to be retinol, vitamin A.1516
Retinol Supports Immune & Reproductive Function
Vitamin A (retinol) can be thought of as the “robustness” vitamin, supporting proper growth and development, immune function, and reproductive function. In pregnancy, vitamin A is required for stem cell differentiation and organ development. Its deficiency is linked to various structural birth defects.1718 Vitamin A deficiency in developing countries is a significant contributor to child mortality.
In men, vitamin A (retinol) is critical for healthy sperm production, so much so that drugs that block the retinol (vitamin A) receptor can act as “male birth control.”19 Without vitamin A, it’s impossible to make sperm.20
In women, retinol supports the implantation of the embryo and helps the embryo and placenta develop properly.21 Retinol is needed by the corpus luteum to make progesterone.
By supporting proper immune function, retinol can protect against autoimmunity, allergies and chronic inflammation caused by inappropriate immune activation.2223
Vitamin A Protects Against Hypothyroidism
Vitamin A is needed to help the thyroid gland take up iodine to make thyroid hormones, convert T4 to T3 (the active thyroid hormone), transport thyroid hormones to cells, and help cells take up thyroid hormones by increasing the number of thyroid hormone receptors. Deficiency can contribute to goitres, Hashimoto’s and hypothyroidism.24
When vitamin A is deficient, the expression of thyroid hormone receptors in the brain is down-regulated. Consequently, T3, the active thyroid hormone, doesn’t work well in the brain when vitamin A is deficient, resulting in low brain energy and poor cognitive function.25
Retinol Enables Healthy Cell Turnover
Retinol maintains the barriers that protect the body from the outside world. It is needed to maintain the gut lining, as well as the mucous barriers lining our eyes, lungs, mouths, skin, and reproductive and urinary tracts. Without adequate vitamin A, these membranes can degenerate, leading to increased susceptibility to infections and symptoms like reduced vision, gastric ulcers and dryness (dry eyes, dry skin, vaginal dryness).
Vitamin A deficiency can contribute to leaky gut, as retinol is needed to constantly replace the cells that line the gut, to increase the number of tight-junction proteins, and to stabilize immune function, which prevents the overproduction of inflammatory cytokines.
Supporting barrier maintenance is part of the reason why vitamin A protects us from infections, as healthy barriers (skin, gut, and lung barriers) prevent the entry of viruses and bad bacteria into the body.
Because it regulates cell turnover and normal cell division, vitamin A deficiency often shows up in fast-renewing tissues, like those on the skin or those making up the gut lining. The impaired cellular turnover in retinol deficiency can lead to acne, and when severe, even certain skin cancers.26
Retinol As a Metabolic Regulator
“Vitamin A supports a wide range of systemic functions, acting much like a hormone […] to regulate the expression of ~300 genes in specific target tissues.”27
Apart from being a building block for the synthesis of the sex hormones, vitamin A itself seems to have a hormone-like regulatory function on the metabolism when it binds to retinol receptors. For example, through its hormone-like signalling, adequate vitamin A can protect against fat gain and insulin resistance.28
Retinol Builds Bones & Teeth
Vitamin A works together with vitamins K2 and D3 to maintain our bones and teeth. Vitamin A is needed for the maturation, “activation” and control of osteoblats and osteoclasts, which are cells that control the growth and remodelling of our bones.29
Diets low in vitamin A can result in thin bones, stunted bone growth, misshapen bones (due to poor osteoblast activity), but also “bony” overgrowths in places where they shouldn’t be (due to poor osteoclast activity).30
In terms of how these vitamins work together:
Vitamin A helps osteoblasts (the “builders”) mature and regulates the activity of both osteoblasts ( the “builders”) and osteoclasts (the “chippers”).
Vitamin D ensures the absorption of calcium and phosphorus from food.
Vitamin K2 directs calcium deposits into bones as opposed to “non-bone” soft tissues, like the arteries.
Vitamins D and K2 enhance the action of the “builder” cells, helping them produce and activate proteins that mineralize bone and produce and maintain type I collagen, bones’ main component.
“Both these vitamins [vitamin A and D], working in close association, play an important part in bone growth-the one influencing the shape, the other the hardness. First vitamin A controls, or at least influences, the activity of the osteoblasts which lay down the soft bone. Vitamin D then attends to its calcification. Vitamin A again steps in and sees that, any superfluous [unnecessary] calcified bone is removed by osteoclastic action.”31
Vitamin A also supports dental health. Retinol is needed for the maturation, “activation,” and control of cells that help create tooth enamel. Retinol deficiency can lead to weak or missing tooth enamel, as well as poor jaw development and teeth that fail to erupt or come in very slowly.323334
Vitamin A exists in two main forms:
Retinol: The animal-based, colourless, active form.
Carotenoids: Plant-based orange, yellow and red pigments (e.g. beta-carotene) in colourful (yellow, orange, red, purple, dark green) fruits and vegetables. Humans have a limited ability to transform carotenoids into active vitamin A (retinol), and factors like hypothyroidism, iron35 deficiency, or certain genetic variations can further interfere with this process. Yellow/orange calluses on hands and feet are a known symptom of hypothyroidism, and are caused by carotenoid accumulation in tissues, as the body fails to convert them to active vitamin A.
While vitamin A deficiency is widely considered a concern only in poverty, when access to foods like milk or meat is unaffordable, the popularization of vegan diets has made it so that retinol deficiency is now a concern in affluent societies, where animal foods aren’t outside of budget. Vegan diets, if not supplemented, are entirely devoid of retinol, while also often lacking in protein, iron and zinc, which are needed to make vitamin A functional in the body.
Since retinol is fat-soluble, the body can store quite a bit of it. A healthy liver can store up to a year’s supply of retinol.36
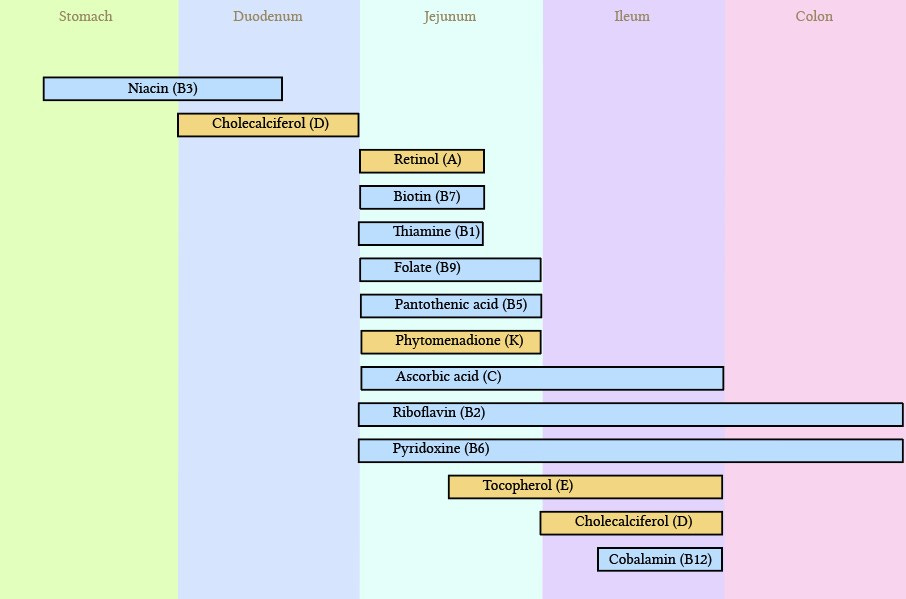
Like most vitamins, retinol is absorbed in the small intestine.
Common Symptoms of Retinol Deficiency:
The most visible signs of vitamin A deficiency can be seen by examining the eyes and skin. In vitamin A deficiency, skin tends to be dry, scaly, bumpy and thick.
Phrynoderma, aka “toad skin” (first two photos) and follicular hyperkeratosis, aka blocked and enlarged hair follicles that create a pebbled skin appearance (last photo), are common manifestations of vitamin A deficiency.
Bitot’s spots, which are foamy deposits on the eyes (3rd and 4th picture), are a sign of vitamin A deficiency-induced eye degeneration, which can progress to blindness if the deficiency isn’t corrected.
Eye Problems and Vision Loss:
Bone and Tooth Deformities:
Skin & Hair Deterioration:
acne, dry or bumpy skin patches (usually on the face, elbows or knees), phrynoderma (“toad skin”), loss of skin elasticity, excessive fine lines/wrinkles, poor wound healing, eczema, hyperpigmentation of the skin (melasma, dark patches over elbows or knees), alopecia (hair loss), enlarged hair follicles, dry, brittle hair (due to inadequate sebum production)4142434445
Hormonal Imbalances:
hypothyroidism, goitre, high TSH, infertility, low progesterone, low testosterone, low DHT, high cholesterol (vitamin A helps convert cholesterol to sex hormones, so in a deficiency the conversion is impaired), miscarriages, poor sperm quality, all sorts of birth defects (when the mother is retinol deficient)46
Immune Dysfunction:
getting sick easily, frequent respiratory, urinary, gastrointestinal and skin infections, autoimmunity, infections that take longer to resolve and are more severe, chronic inflammation (vitamin D cannot exert its anti-infective, anti-autoimmunity effects when vitamin A is deficient. Vitamin A “activates” vitamin D, and restores the function of defective vitamin D receptors)4748
“Dryness”:
dry eyes, dry skin, dry, cracked lips, vaginal dryness, inability to make protective “mucus” in the lungs (leading to more respiratory infections)
Impaired Digestive Lining Integrity:
leaky gut, stomach ulcers, mouth ulcers, oral leukoplakia
Other:
On a blood test:
Plasma retinol < 1 μmol/L indicates that vitamin A levels are low. Plasma retinol < 0.70 indicates a deficiency.
This test is not perfect. Inflammation (indicated by high CRP) can cause a low reading by lowering retinol-binding protein, even if the body has enough vitamin A.
Testing plasma retinol & retinol binding protein levels together can create a better picture of retinol status.
Retinol Binding Protein (RBP) < 40 mg/L indicates poor retinol status, and <20 mg/L indicates a more severe deficiency.
CRP should be tested to see whether high inflammation is messing up the accuracy of the retinol tests.
Factors That Predispose to a Vitamin A Deficiency:
Lots of sun exposure. Heat and UV light deplete vitamin A.5152
A history of vegan diets. Retinol is only found in animal foods.
A history of extremely low-fat diets. Retinol is a fat-soluble vitamin. Extremely low-fat diets can interfere with its absorption, in part by lowering the expression of gut proteins that help with retinol uptake.53
Very high-fibre diets. Excessive fibre can act like an “anti-nutrient,” binding fat-soluble vitamins and preventing their absorption.
A high metabolic rate. A high metabolic rate increases the requirement for vitamin A.
“There is an increased need for vitamin A in hyperfunction of the thyroid gland, the blood content of vitamin A in human beings suffering from hyperthyroidism falling even to zero despite adequate intake.”54
Bariatric surgery (duodenal switch). Some types of bariatric surgery (surgeries that modify the digestive tract to limit how much food an obese person can eat) are also meant to induce nutrient malabsorption. Certain variations of this surgery, particularly duodenal switch surgery, can result in vitamin A deficiency by interfering with fat absorption. People who’ve undergone such a surgery might require long-term vitamin A supplementation.55
Fat malabsorption (due to gallbladder, pancreas or liver problems). The inability to create and release bile (due to liver or gallbladder problems, such as gallstones or cholestasis) and the inability to create lipase (a digestive enzyme released by the pancreas that helps with fat digestion) can interfere with vitamin A absorption.
Supplemental ox bile (for those with bile flow issues, or those lacking a gallbladder) or supplemental lipase (when pancreatic digestive enzymes are deficient, for example, in cystic fibrosis, when the release and function of lipases is reduced due to hypothyroidism, or in digestive disorders like IBD) can help overcome this.56 Supplemental thiamine (vitamin B1) can often restore the pancreas’s ability to release digestive enzymes (including lipase).
Liver disease (high ALT, AST, bilirubin). The liver is the primary storage organ for vitamin A, and liver disease can limit the liver’s ability to store it.
Zinc deficiency. Zinc is needed to absorb, store, and convert retinol to its bioactive derivatives: retinal and retinoic acid. Zinc deficiency can lead to both vitamin A deficiency symptoms (as vitamin A can’t be converted to its bioactive form) and vitamin A toxicity symptoms. This is because excess free retinol in the blood can be very reactive and destructive. Zinc prevents this by helping to make proteins that “chaperone” retinol in the blood and bind retinol in the liver in its storage “for later” form.57 These proteins are aptly called “retinol binding proteins.” Iron and protein are also involved in the creation of these proteins, and iron or protein deficiency can similarly interfere with vitamin A distribution.
Vitamin B3 deficiency. Vitamin B3 (niacinamide) converts to NAD+ in the body. NAD+ is necessary for mitochondrial energy production and is also involved in converting retinol to its bioactive forms. Low NAD+ (and a low energy state in general, such as hypothyroidism) can lead to “paradoxical” symptoms of both vitamin A deficiency and vitamin A toxicity. The conversion process goes like this: retinol —> retinaldehyde —> retinoic acid. Both of these steps are NAD+ dependent. As the conversion of retinol to its bioactive forms is impaired, vitamin A can’t perform its functions in the body. At the same time, retinaldehyde can be toxic if it builds up in the body due to vitamin B3 and energy deficiency.58
Alcohol intake. Alcohol and vitamin A have something in common. The same enzymes that detoxify alcohol (ADH & ALDH) are also involved in converting retinol to its active metabolites. Alcohol can overwhelm these enzymatic pathways, once again, leading to the “paradoxical” outcome of: “vitamin A deficiency & vitamin A toxicity at the same time.” By damaging the liver, alcohol is also known to deplete vitamin A in the livers of alcoholics, without which, the liver can’t regenerate well.59
“Ethanol, while promoting a deficiency of vitamin A also enhances its toxicity as well as that of b-carotene.”60
Accutane (isotretinoin) use. Accutane is often thought of as “vitamin A,” but it is not. It’s a synthetic derivative of vitamin A that the body doesn’t produce naturally. It’s not able to perform many of the functions that real vitamin A can, while also blocking the conversion of retinol to its bio-active forms, creating a functional vitamin A deficiency. Accutane often comes with “side effects” like night blindness, severe fatigue, sexual dysfunction, osteoporosis, IBS, etc - classic signs of vitamin A deficiency. Chris Masterjohn PhD refers to Accutane as “anti-vitamin A,” and has brought up a case study where patients who developed depression on Accutane (due to the anti-vitamin A effect of the drug) saw their depression disappear when they were taken off Accutane and put on 10,000-12,000 IUs of real vitamin A for about one week.616263
Inflammation (high CRP, IL-6). Chronic inflammation, for example, due to gut infections, can interfere with the synthesis of the retinol binding protein. This protein helps to transport vitamin A from the liver to the different tissues that need vitamin A for their proper function. Bacterial endotoxin, by messing with the liver’s ability to make retinol binding proteins and distribute vitamin A, can lead to a functional vitamin A deficiency (and excess vitamin A accumulation in the liver).6465
Activated charcoal and ginger can be helpful in dampening bacterial endotoxin-induced inflammation.
Early weaning (in babies), because babies have a limited capacity for storing retinol and rely on breast milk for a consistent supply of it.
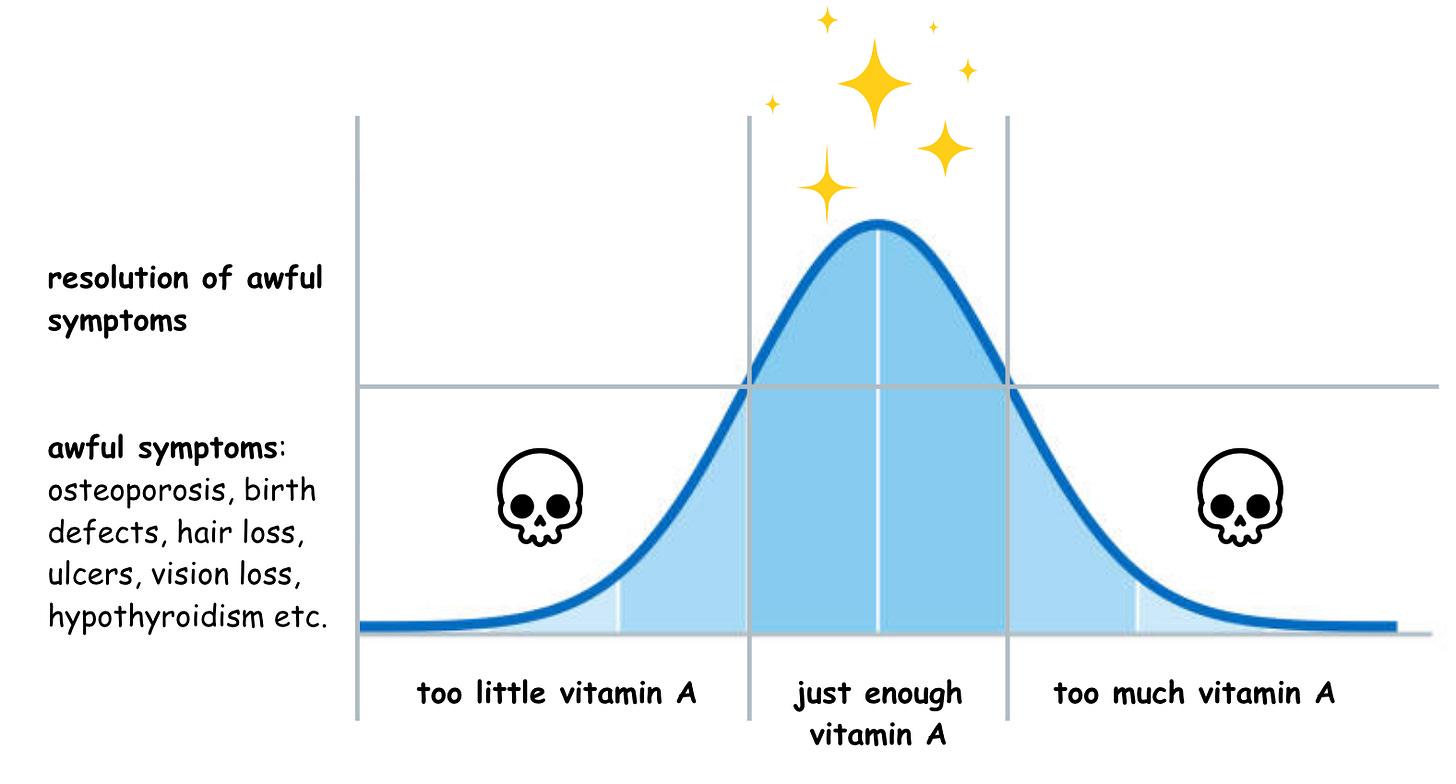
Vitamin A Toxicity - Retinol: A Double-Edged Sword
An excess of vitamin A can be just as detrimental as a deficiency, leading to virtually all of the same symptoms. Just as not having enough vitamin A can lead to osteoporosis, weak bones, weak teeth and bone spurs…too much vitamin A can also lead to osteoporosis, weak bones, weak teeth and bone spurs (by over-activating the cells that tear down bones and teeth, messing with the process of bone turnover). 6667
Just as too little vitamin A can lead to hypothyroidism, so can an excess of it. Excessive vitamin A has many anti-thyroid properties, including interfering with thyroid hormone synthesis. High-dose vitamin A has been used to reverse hyperthyroidism due to its anti-thyroid properties.6869
Just as too little vitamin A can cause the hair to fall out and the skin to “fall apart,” so can an excess of it.
Just as too little vitamin A can make a person more prone to infections, so can an excess, in part by interfering with the function of vitamin D.
And so on…
With vitamin A, more is not better, and excessively supplementing vitamin A or eating large amounts of liver or fish liver oil can rapidly “over-correct” a deficiency and launch a person into vitamin A toxicity territory.
How to Avoid Vitamin A Toxicity
The main way to avoid vitamin A toxicity is to steer clear of cod liver oil supplements.
The recommended daily retinol intake is 900 micrograms for men and 700 micrograms for women. The requirement increases to 750 mcg in pregnancy, and 1,300 mcg when lactating.70 The “tolerable” daily dose for adults is 3,000 micrograms/day. Exceeding this regularly, especially through something like cod liver oil (one tablespoon contains over 4,000 mcg), can lead to toxicity. With vitamin A, more is not better.
“One tablespoon of cod liver oil contains approximately 4,080 ug of retinol (vitamin A) and 34 ug (1,360 IU) of vitamin D. Since the general dietary reference intake of vitamin A is only 900 ug per day for adult men, 700 ug per day for women, and 3000 ug per day as the tolerable upper intake level, the regular intake of cod liver oil as a regular supplement can result in harmful levels of vitamin A accumulating in the liver and is sufficient to cause hypervitaminosis A, which is associated with various symptoms such as blurred vision, changes in consciousness, skin and hair changes, liver damage, among many others.”71
Over-consuming liver (which usually means eating it more than once per week) can also cause vitamin A toxicity.
A Low Metabolic Rate Predisposes to Vitamin A Toxicity
High thyroid function = increased tolerance (and need) for vitamin A
Low thyroid function* = decreased tolerance
“In the presence of hypothyroidism […], everything is dangerous” - Dr. Ray Peat
*Other factors that interfere with energy production (e.g., excess estrogen, deficiency of the B vitamins, especially B1 and B3, hypoxia, and mitochondrial toxins) also lower the tolerance for vitamin A. Any person with a depressed metabolic rate should start with a moderate retinol intake and increase gradually if symptoms persist.
The vast majority of people (especially sick people) are in a low-energy state (whether due to hypothyroidism, excess estrogen, environmental pollutants, or missing nutritional cofactors). A depressed metabolic rate slows down the use of vitamin A, increasing its accumulation. As such, in a low-energy state, it’s easier to reach the toxicity threshold.
Cod liver oil + a diet that’s high in vitamin A-rich foods (dairy, liver pate, eggs) + a low metabolic rate = a recipe for vitamin A toxicity.
You can probably double that likelihood in anyone who drinks alcohol, is deficient in minerals and B vitamins, and has poor liver health.
Extreme and Non-Contextual Dietary Advice is to Blame for the Vitamin A Confusion
Context matters when considering vitamin A or cod liver oil supplements. Dr. Weston Price used cod liver oil to reverse severe tooth decay in malnourished children. Children have higher metabolic rates than adults, and the kids that Dr. Price focused on were, again, severely malnourished. That context doesn’t apply to most people today eating a varied omnivorous diet.
On a well-rounded omnivorous diet, one that contains dairy, eggs and some organs, vitamin A deficiency is rare.
Certain nutritional outlets, like The Weston A. Price Foundation (which postdates Dr. Price and adds its own spin when interpreting his work), or Morley Robbins’ “Root Cause Protocol” (inspired heavily by recommendations from the Weston A. Price Foundation), promote the broad use of cod liver oil supplements. As mentioned, for most people, this is unnecessary and potentially harmful. Chronic sickness in adults is frequently downstream of metabolic suppression, meaning that their tolerance threshold for vitamin A is already low.
Lately, there has been an uptick in alternative health accounts and publications swinging in the other direction, blaming all diseases on vitamin A, calling it a “poison” and a “toxin.” This sentiment started gaining quite a bit of traction back in 2023, which is no surprise to me as the “wave” that the alt health world embraced in the year or two before that was all about Morley Robbins’ “Root Cause Protocol” and his conviction that “everyone is vitamin A deficient” and should supplement it.
Generalized advice to take vitamin A or cod liver oil can easily result in the development of vitamin A toxicity. If this happens, it’s not uncommon for a person to become convinced that “vitamin A is a poison,” leading them toward total vitamin A avoidance, eventually making them sick “in the opposite direction.”
Unless you’re a recovering vegan, get plenty of sun exposure year-round, have a high metabolic rate, and maybe can’t absorb fats well, you probably do not need cod liver oil, daily beef liver capsules, or any other sort of supplemental vitamin A.
Topical retinol (in skincare) can also contribute to systemic toxicity if overused.72
A nutrient-dense diet with animal foods, like eggs, dairy (especially goat and sheep), and liver (1-4 times per month, as per cravings) should provide sufficient vitamin A for the average person.
Keeping the metabolic rate high, getting sun exposure, avoiding cod liver oil, and consuming adequate vitamins B3, vitamin E (which helps prevent the oxidation of the unsaturated vitamin A) and zinc, protect against vitamin A toxicity7374.
Who Might Benefit from Extra Vitamin A
Here are the types of people who might benefit from vitamin A supplements (or from short-term use of cod liver oil):
People with malabsorption disorders (for example, those missing part of the digestive tract after surgery).
People with very high metabolic rates (either naturally or due to T3 supplementation), who also get plenty of daily sun exposure.
People who have been vegan for a long time and are now experiencing severe symptoms of vitamin A deficiency, like tooth decay or infertility.
People (especially children) who are extremely malnourished due to homelessness or poverty.
For most other people (those who don’t fit the above categories), vitamin A supplements are not necessary and even dangerous.
Testing For Vitamin A Toxicity
The following markers can indicate toxicity:
Elevated serum retinyl ester concentrations (> 7.5% or 5% of total vitamin A for adults and children, respectively) in fasting blood samples75
Plasma retinol > 3 μmol/L
Supplemental markers: Elevated liver enzymes, high blood calcium76
Treating Vitamin A Toxicity
Vitamin A toxicity is slow to resolve because the body recycles stored vitamin A for repeat use.77
If vitamin A toxicity is confirmed, then following a low vitamin A diet for 1-2 months (or until blood levels normalize) might be a good idea.
Most of the foods eaten on a low vitamin A diet are white (or off-white, but never orange, green, red, or another pretty colour) and lean (since retinol is mostly stored in fat).
Such a diet prioritizes “colourless” fruits and vegetables (peeled pears, peeled apples, peeled white peaches, lychees, cherimoyas, bananas, cauliflower, celeriac, parsnips, lotus root, daikon, peeled white potatoes), oats, sourdough bread/nutritional yeast, white rice, molasses, coconut oil, some seafood (scallops, cod), non-fat dairy and muscle meats (steak, chicken breast). It excludes full-fat dairy, butter, liver, fatty fish, fish liver oils and colourful fruits and vegetables.
Vitamin E supplements can also help treat vitamin A toxicity by offsetting the toxicity of excess vitamin A.7879
Conditions That May Improve With Adequate (But Not Excessive) Retinol Intake:
Acne and “aged” skin80
Alzheimer’s disease (reduction of amyloid plaque in a mouse study)81
Anemia82
Cavities83
Cervical neoplasia84
Depression85
Fibrosis88
Hyperkeratosis/keratosis pilaris89
Hypothyroidism90
IBD91
Infections (including measles, diarrheal, and general respiratory infections in children)929394
Infertility95
Leukemia (acute promyelocytic leukemia)96
Lupus97
Macular degeneration98
Melasma/hyperpigmentation99
Menstrual irregularities
Multiple sclerosis100
Night blindness101
Osteopenia/osteoporosis (but is worsened by excess vitamin A)102
Poor sperm quality103
Psoriasis104
Type 1 Diabetes (prevented the development of T1D in mice)107
Food Sources of Retinol:
“Milk and milk products must be perfectly protected against light; otherwise, significant amounts of […] vitamin A (retinol) […] will be lost and food quality will deteriorate.”108
Vitamin A (retinol) is sensitive to UV light. This means that keeping foods high in retinol out in the sun, or in general, exposing them to bright light (for example, keeping milk in clear bottles or leaving cheese out in the sun) can destroy the vitamin A in these foods.
Liver ⭐️ - potent, use sparingly
Eating too much liver poses the same risk as cod liver oil. Having liver once per week, for a healthy person, is enough. A “sicker” person might only tolerate liver once a month or a smaller serving.
50 g of beef liver = ~3,870 mcg of retinol
50 g of chicken liver = ~2,148 mcg of retinol
Dairy
Full-fat goat or sheep milk, cheese, yogurt, and butter
Eggs
Eel
The retinol RDA (900 micrograms) can be met fully by each of the following: 10 grams of beef liver, 25 grams of chicken liver, 70 grams of eel, or 2 litres of goat milk.
My Preferred Retinol Supplements:
I generally wouldn’t recommend retinol supplements, except for strict vegans.
A strict vegan might benefit from a supplement that contains all of the fat-soluble vitamins in reasonable amounts, such as IdeaLabs EstroBan (4 drops of the product meets the retinol RDA).
Now Onto the B Vitamins…
A Word on B Vitamins and Why We Shouldn’t Treat Them Like a Monolith
I want to share a word on the B vitamins before I jump into thiamine (B1), our first B vitamin.
Of the 13 known “true” vitamins, 8 are part of the B vitamin class. These vitamins are part of the B complex.
If you’ve ever had a bad experience with a B complex supplement, this does not rule out a deficiency in one or more of the B vitamins.
While all of the B vitamins share some similarities, like water-solubility and being involved in cellular energy production, I feel it is necessary to really, really emphasize that each is a unique compound with specialized functions. Each is also chemically distinct.
For example, thiamine has sulphur in its structure, while vitamin B12 (cobalamin) contains cobalt as its core component. Some are heat-stable, others are not. Some have no known toxicity thresholds, while others should be used carefully, as too high a dose can cause adverse effects like liver injury. Some of these vitamins are also antagonistic. For example, too much B6 can worsen a B1 deficiency. And so on.
And so, a person might desperately need more vitamin B2 or B5 while simultaneously needing less B6 or B9. Similarly, avoiding vitamin B2 because of a bad reaction to vitamin B3 would be kind of like avoiding cherries because bananas gave you indigestion. They might have some things in common, but they are not the same thing.
Why Are All These Different Compounds Classed as “B” Vitamins?
So why are all of these unique compounds assigned the letter “B”? The answer to this question has to do with the history of their discovery.
In short, there was some initial confusion around the time when these vitamins were being discovered, leading scientists to think that a yeast that contained multiple B vitamins only had one type of vitamin in it. As they realized that this yeast compound that they initially called “water-soluble B” was more than one type of “water-soluble B,” they just started assigning these vitamins numbers instead of new letters, which helped to keep track of the fact that they all came from that yeast.
Why not rename these compounds then? Probably in part because once something is named, it’s harder to back track and fix the name than to just roll with it and probably in part because it didn’t seem like a serious enough thing to correct.
A Deeper History of “Water-Soluble B”
In the 1920s, a “vitamin” that became known as “water-soluble B” was extracted from yeast. The only other vitamin that was known at the time was “fat-soluble A,” aka, vitamin A.
It was first assumed that “water-soluble B” is the same compound as the “anti-beriberi factor” that Funk isolated.109 However, researchers soon realized that giving animals “water-soluble B” could cure some diseases that the “anti-beriberi factor” could not.110
Soon, it was evident that the yeast extract contained not one, but multiple vitamins.
As scientists isolated each new compound from the “water-soluble B” preparation, they started assigning numbers to these cascading discoveries, rather than assigning them their own letters. And so, we ended up with vitamins B1, B2, B3, and so on. This numerical system then became the template for classifying every vitamin that was water-soluble and involved in energy metabolism as part of the "B group," regardless of how different these compounds were from each other. If vitamin discovery had unfolded differently, these vitamins may have been named vitamins X, Y and Z instead.
We Assigned a “B” to a Bunch of Different Compounds, and Now Everyone is Confused
The way the B vitamins are named makes it harder to grasp that B1, B2, and B12 are as fundamentally different from each other as vitamins A, D, and K.
Think of it this way:
Vitamins A, D, and K all work synergistically and support each other's functions (similarly to how the B vitamins work together to support energy metabolism).
Vitamins A, D, and K are all fat-soluble and involved in bone turnover.
By the B vitamin naming logic, vitamins A, D and K could easily be called fat-soluble A1, A2 and A3, and sold as an "A complex" in a parallel universe.
Yet, since we’ve assigned them different letters, nobody struggles to understand that the functions of vitamin A (supporting eye and skin health) differ from those of vitamin D (calcium absorption, immune regulation) or vitamin K (blood clotting, calcium distribution).
While a B-complex supplement is a great choice in many cases, the choice to supplement B vitamins should be made with the awareness of the distinct qualities of each in mind.
I want you to keep this in mind when reading and applying the rest of this article series.
Vitamin B1 (Thiamine)
The anti-fatigue, anti-diabetic, brain-and-nervous-system energizer.
Predominant deficiency symptoms:
fatigue, dysautonomia (POTS), cognitive and memory impairments, slow digestion, difficulty focusing, depression, neuropathy/nerve problems (especially in the hands and feet), carbohydrate intolerance (high blood sugar, diabetes, fat gain)
The Importance of Thiamine:
Thiamine Is Needed To Turn Foods (Especially Glucose) Into Energy
It seems that symptoms of vitamin B1 deficiency can be nearly endless. Why? Because without B1, you can’t turn food into energy. Behind virtually any illness, especially any chronic metabolic illness, like type 2 diabetes, Alzheimer’s disease, Parkinson’s disease, cancer, obesity and chronic fatigue syndrome (CFS), lies the inability to effectively turn fuel, especially glucose, into energy (ATP). Your body runs on energy, so if you can’t turn the foods you eat into energy, all the systems and functions in the body take a hit.
“Cellular respiration” is the process through which cells turn glucose into energy. Most of the energy created in this process is created by the mitochondria.
Thiamine, via the enzyme pyruvate dehydrogenase (PDH), links glycolysis, the first stage of cellular respiration (which takes place in the cytosol), to the Krebs cycle, the second stage of cellular respiration (which takes place in the mitochondria). In essence, thiamine is the mitochondrial “bridge” for glucose.
If glucose makes it through all three stages of cellular respiration, you make 36-38 units of ATP (energy). However, if glucose fails to enter the Krebs cycle (because thiamine is deficient and the “bridge” to the mitochondria isn’t established), it is instead converted to lactate, yielding only 2 ATP (vs. 36-38 when fully metabolized). In other words, thiamine enables the burning of glucose for energy.
As a cofactor for multiple enzymes involved in oxidizing fuel, thiamine has additional roles in burning fats and proteins (BCAAs). It also helps us regenerate and increases the activity of our key antioxidant, glutathione.111
Thiamine Protects Against Cancer and Diabetes
In thiamine deficiency, glucose is excessively “fermented” into lactate instead of being turned into energy. Excess lactate is a metabolic toxin and energetically costly for the body to process. Cancer is characterized by the overproduction of lactate due to impairments in the respiratory chain (a phenomenon called “The Warburg Effect”). Lactate itself is a driver of cancer, promoting undifferentiated cell division.112
Some research shows that high-dose thiamine can suppress cancer progression by restoring the function of the thiamine-dependent enzyme pyruvate dehydrogenase (PDH),113114 as well as other thiamine-dependent enzymes in the Krebs cycle, like α-ketoglutarate dehydrogenase (α-KGDH). This can help oxidize glucose fully, preventing the accumulation of lactate.
Thiamine, being the chief “glucose supervisor,” helps to burn glucose for energy, use glucose to make antioxidants, and protect against glycation (by preventing the build-up of glucose intermediates in the cell). In doing so, thiamine is also highly anti-diabetic, protecting against the development and complications of diabetes.115
By supporting energy metabolism, glucose burning, and liver health, thiamine has additionally been shown to lower triglycerides and total cholesterol levels.116
Thiamine is Needed to Power the Brain and Nervous System
The brain and nervous system are confined to glucose as their main fuel source. They can’t switch to running on fats. Since glucose can’t be turned into energy without thiamine, thiamine deficiency strongly manifests as symptoms of energy deficiency in the brain and nervous system. These include ADHD, memory problems, cognitive impairments, dysautonomia, mood disorders, irritability, fatigue, nerve pain, and nerve degeneration.
Thiamine supports healthy nerve function by maintaining the myelin sheath. It is needed for the metabolism and function of brain cells. Thiamine improves nerve transmission in the brain and maintains healthy “brain chemistry.” It is needed to synthesize and release neurotransmitters (including dopamine,117 which is low in depression, ADHD, dementia, Alzheimer’s disease and Parkinson’s disease) and DNA, and to help the brain take up neurotransmitters, including the very calming neurotransmitter GABA. Depression can be caused by a thiamine deficiency.118 Severe depression is a known symptom of “dry beriberi.”119
By powering the central nervous system, thiamine also improves exercise tolerance, endurance, balance and grip strength.
If eating carbs isn’t helping you overcome your fatigue, brain fog or hypothyroidism, but is instead making you gain a lot of fat or worsening your fatigue and brain fog, you are likely thiamine deficient.
Thiamine is Needed for Good Digestion
Thiamine is needed for the release of digestive enzymes, like trypsin, amylase and lipase. Thiamine deficiency can lead to more downstream deficiencies by lowering our ability to absorb vitamins and minerals from the foods we eat.120 Cases of protein, fat or carbohydrate malabsorption can be caused by thiamine deficiency.
Some cases of SIBO can be caused by thiamine deficiency. This is because thiamine is needed to maintain gut motility (preventing constipation), to release stomach acid (which kills bacteria in foods), to absorb fats, carbs and proteins in the small intestine (and stop bacteria from feeding on them), and to run the migrating motor complex which “sweeps” the gut between meals, helping to prevent the overgrowth of bacteria.121
Thiamine protects against leaky gut by helping intestinal cells make energy, so that they can power their growth and repair.122
Thiamine deficiency can also contribute to gut dysbiosis, lowering the levels of helpful butyrate-producing bacteria that rely on thiamine for survival.123
Some Forms of Thiamine Can Chelate Mercury (and Might Improve Autism Symptoms)
TTFD (thiamine fetrahydrofurfuryl disulfide) is a synthetic, fat-soluble, and very potent form of thiamine, created to better treat severe beriberi. It was synthesized in Japan from allithiamine, its naturally occurring counterpart found in garlic, which contributes to garlic’s distinct smell. It also turned out to be a powerful mercury chelator.
Due to the large quantities of seafood consumed, Japan struggles with high rates of mercury exposure and toxicity. Decades after TTFD was first synthesized, a group of Japanese researchers, in an effort to investigate new approaches to mercury chelation, found that TTFD can act as a potent mercury chelator, moving mercury out of the body by depositing it in hair.124
This function is specific to the TTFD form of thiamine because its chemical structure contains a compound called furfurylmercaptan. The word “mercaptan” comes from the Latin “mercurium captans,” meaning seizing or capturing mercury.125
Mercury is considered one of the many contributing factors to autism. In a small study on 10 autistic children, 8 had clinical improvements in their symptoms of autism spectrum disorder after using 50 mg of TTFD twice daily for 60 days.126
Nowadays, the term “mercaptan” is obsolete, being replaced by the term “thiol,” which you might recognize from my article “How to Safely Detox Heavy Metals.”
In that article, I wrote about how many of the thiol-containing metal chelators, like ALA and DMPS, can pose the risk of metal redistribution. This is because most chelators attempt to remove metals via the urine and feces. This creates many opportunities for reabsorption and redistribution if the metal is let go of prematurely.
What distinguishes TTFD and similar fat-soluble mercaptan-containing thiamine derivatives, as per the research conducted in Japan, is that they do not increase the levels of mercury and other toxic metals in the urine or feces. Instead, they deposit mercury in hair follicles and use hair growth as the primary elimination pathway. These researchers also concluded that the bonds between furfurylmercaptan and mercury remain stable, lowering the risk of redistribution.
“Hair is the main route by which mercury is excreted in the human body by TTFD […] Considering that the side chains of TPD, TTFD, TATD, etc., change the originally water-soluble substance B into a fat-soluble substance, metals in the body that bind to these side chains become fat-soluble substances, and are likely to be excreted in body hair rather than in urine or feces."127
(quote translated to English from the original paper published in Japanese)
The body has a limited ability to store thiamine, as it is a water-soluble vitamin that gets peed out easily. It has a half-life of about 12 hours128 and can be fully depleted from the body in 2-3 weeks if the diet doesn’t provide it or if it can’t get absorbed. All types of stressors accelerate its use and expedite its depletion.
Psychological stress, exercise, pregnancy, breastfeeding, a high metabolic rate, sickness, inflammatory diseases, diabetes, and excessive urination can deplete thiamine quickly (sometimes in a day), increasing the need for it.
Alcohol intake (especially chronic) and diets full of refined carbs (white sugar, white flour, white rice) rapidly deplete thiamine.
Anything that lands a person in the ICU (like severe burns or sepsis), and especially head injuries, will deplete thiamine extremely rapidly, as the body relies on thiamine to make heaps of energy to heal.
Increased cognitive demands (studying, playing chess, or being smart in general) boost the brain’s energy demands, skyrocketing the amount of glucose that it burns. This can accelerate thiamine use, hastening its depletion.
Common Symptoms of Thiamine Deficiency:
Thiamine deficiency leads to “energy failure” in the whole body, but especially in the brain and nervous system, leading to fatigue, memory loss, dysautonomia, cognitive decline and weakness.
While there aren’t “easy” skin or hair changes that you can use to spot this deficiency, tingling in the hands and feet, feeling wobbly and losing balance, always feeling tired or irritable, being more forgetful, constipation and feeling “dumber” can be key signs.
Impairments in Carbohydrate Metabolism:
gaining fat easily when eating carbs, sweet cravings, lactic acidosis, type 2 diabetes, high blood sugar, obesity
“An increased consumption of processed food in the form of simple carbohydrates, not supplemented with adequate levels of thiamine, has been named “high calorie malnutrition”. […] At least 29% of obese subjects that will undergo bariatric surgery have been reported as thiamine deficient.”129
Nervous System:
dysautonomia (dizziness/vertigo, muscle weakness), reduced reflexes, difficulty swallowing, seizures, hands and feet that “fall asleep” easily and go numb (especially at night), loss of tendon reflexes (for example, tendon reflexes are tested when a doctor hits the knee with that little hammer), neuropathy (including diabetic neuropathy), loss of muscle function in lower legs, involuntary eye movements, eye paralysis, loss of smell, voice or hearing, lack of coordination/poor coordination, worsening of symptoms when exposed to sunlight/UV light, low vagal tone/vagus nerve dysfunction (thiamine is involved in synthesizing and releasing acetylcholine, and itself has cholinergic properties), insomnia130131132133
“Beriberi is the popular name for a group of disorders due to thiamine deficiency. […] When afflicted patients in Sri Lanka […] were asked to move, they responded in the Sinhalese language with “beriberi,” which translates to ‘I cannot. I cannot.’”134
Low Energy Availability:
fatigue (including CFS), muscle atrophy, sleep disturbances, exercise intolerance (and leg swelling from exercise)
Mood & Mental Health:
Brain Hypo-Metabolism & Cognitive Impairments:
ADHD, brain fog, confusion, general intellectual decline - including loss of verbal and mathematical skills, inability to learn new things or make new memories, distractibility/short attention span, difficulty finding words, dementia & poor memory, loss of memories, speech difficulties, difficulty finding words, false memories (confabulation)
Digestion:
constipation, gastroparesis, loss of appetite, nausea, vomiting, abdominal pain, low stomach acid (discomfort in the stomach when eating, excessive burping, feeling full quickly when eating), IBS, SIBO, pancreatitis
Cardiovascular:
edema, rapid heart rate, cardiomyopathy (symptoms of it can include swelling in the legs, shortness of breath and fatigue), chest pain, fluid in lungs, strokes, low blood pressure
Low CO2:
sleep apnea, shortness of breath (also with exercise), altitude sickness
Other:
estrogen dominance (vitamin B1 helps the liver eliminate estrogen), heavy menstrual bleeds, bleeding between periods, megaloblastic anemia, hoarse voice, garlic and pork cravings
“While studying vaginal and cervical cytology smears for a diagnosis of uterine cancer, […] over two-thirds of the 150 cases proven to be cancer showed evidence of abnormally high endogenous estrogenic activity. […] thiamine and riboflavin [vitamin B2] are essential in the metabolism of estradiol by liver slices. […] the liver loses its ability to inactivate estrogen in vitamin B-complex deficiency. […] The amount of estrogen inactivated by the liver could be controlled at will by withholding the vitamin B complex or by restoring it to the diet. […] errors of diet leading to persistent or intermittent deficiency of such elements as thiamine might cause a persistent estrogenic growth.”137
On a blood test:
“Thiamin deficiency increases concentrations of both pyruvate and a-ketoglutarate in whole blood or plasma, and of methylglyoxal in urine and cerebrospinal fluid”138
eTKac (erythrocyte transketolase activity coefficient):139 ← the main test for spotting a thiamine deficiency
eTKac <1.15 - low risk of deficiency
eTKac between 1.15 - 1.25 - moderate risk of deficiency
eTKac > 1.25 - high risk of deficiency
eTKac > 1.40 - beriberi likely (severe deficiency)
High lactate levels (> 2 mmol/L) can signal a thiamine deficiency
High pyruvate levels (> 1.0 mg/dL) can signal a thiamine deficiency
High α-Ketoglutarate levels (> 5–10 µmol/L) can signal a thiamine deficiency
High lactate-to-pyruvate ratio (> 25:1 suggests thiamine deficiency) can signal a thiamine deficiency
MCV > 100 fL (might also indicate a B12 or B9 deficiency)
You can also test the level of thiamine in the blood, but this is not an accurate marker of thiamine status. The above proxy markers can be more conclusive.
Factors That Predispose to a Vitamin B1 Deficiency:
“Classic deficiency syndrome (beriberi) remains endemic in Asian populations consuming polished rice diet. Globally, alcoholism, chronic renal dialysis, and persistent nausea and vomiting after bariatric surgery are common precipitants. High carbohydrate intake increases the need for B1.”
- “Sleisenger and Fordtran's Gastrointestinal and Liver Disease- 2 Volume Set: Pathophysiology, Diagnosis,” Management 11th Edition: by Mark Feldman MD, Lawrence S. Friedman MD and, Lawrence J. Brandt MD
High carbohydrate diets (that are low in thiamine). This doesn’t mean that high-carb diets are bad. However, since thiamine is used to turn carbs into energy, if you give the body lots of carbs without lots of thiamine, you can deplete thiamine quite quickly. Severe thiamine deficiency (beriberi disease) was first identified in cultures that eat a lot of white rice (a carb source that lacks thiamine). If you have a history of eating lots of “nutrient-poor” carbs, like white rice, white sugar, candy, white bread, white flour, or Coca-Cola, you likely need more thiamine (especially if presenting with symptoms of thiamine deficiency).
“In malnourished people, high doses of glucose result in acute thiamine deficiency.”140
Drinking alcohol (especially chronic alcohol intake). Alcohol interferes with the absorption of thiamine by injuring the gut lining. Alcohol also breaks down thiamine in the brain and inactivates the enzyme that converts thiamine to its bioactive form (thiamine pyrophosphate). Wernicke-Korsakoff syndrome is a type of dementia that develops in alcoholics due to thiamine deficiency. It is characterized by personality changes (such as irritability and anhedonia), loss of memories, inability to form new memories, and a general decline in cognitive abilities.141
Severe under-eating. States of under-nourishment accelerate the rate of thiamine loss.142
Head injuries. An injured brain consumes a tremendous amount of glucose to power its repair. This rapidly uses up thiamine and can deplete it quickly.143
Chronic stress. Anything that places more energetic demands on the body depletes thiamine.
E.Coli infections interfere with the function of intestinal thiamine transporters.144
Eating lots of raw fish and raw shellfish. Raw seafood contains thiaminases (compounds that destroy thiamine).145 Eating lots of sushi (which contains both raw fish and white rice, two foods that can deplete thiamine) can predispose to thiamine deficiency.
Drinking lots of tea and coffee. Black tea, green tea, horsetail tea and coffee contain thiaminases.146
Eating lots of chocolate or cacao. Theobromine, found in chocolate, can inactivate thiamine.147
Cognitively-demanding jobs. When you think hard, your brain uses up a ton of glucose to generate the energy needed to sustain these cognitively demanding tasks. This can rapidly deplete thiamine if you’re on a low-thiamine diet.
Chronic vomiting and/or diarrhea (Hypermesis Gravidarium, IBS). Induce thiamine loss.
Nicotine use. Some experiments suggest that it can reduce thiamine uptake by pancreatic cells,148 interfering with the release of digestive enzymes.
Metformin use. Metformin can interfere with thiamine uptake by various tissues. There are cases of lactic acidosis linked to metformin use.149
Other drugs that can lead to a deficiency: Famotidine, Phenformin, Chloroquine, Hydroxychloroquine, Phenytoin, and Verapamil.150
Metronidazole (Flagyl) use. Flagyl is an antibiotic, often prescribed for bacterial vaginosis. Some research shows that it can convert to a form of pseudo-thiamine that can act like “anti-thiamine” in the body.151
Diuretic use. Thiamine is water-soluble and can be excessively lost in urine.
PPIs. Proton pump inhibitors reduce thiamine absorption.
Folate deficiency. Animal experiments suggest that folate (vitamin B9) helps with the absorption of B1.152
Adverse vaccine reactions (for example, to Gardasil): Vaccine-induced POTS/dysautonomia is likely caused by thiamine depletion due to residual thiaminases (thiamine-destroying enzymes) found in certain vaccine formulations.153
History of diets lacking pork and whole, fermented grains (like sourdough). Since these are two of the main sources of thiamine in most modern diets, cutting these out can lead to a thiamine deficiency. Some people following a grain-free paleo diet (especially if excluding pork) start showing symptoms of thiamine deficiency.
High-dose B6 supplements. Vitamin B6 is antagonistic to vitamin B1 and can deplete it. Neuropathy from vitamin B6 supplements is likely just a B1 deficiency.
Conditions That May Improve With Vitamin B1:
ADHD154
Autism155
Constipation158
Depression159
Dysautonomia/POTS160
Ehlers-Danlos Syndrome (EDS)161
Fibromyalgia162
Hypoglycemia (thiamine helps the liver store glycogen)163
IBD (relieved fatigue)164
Infertility & poor sperm quality165
Insomnia/hypersomnia (oversleeping)166
Leigh’s syndrome167
MCAS168
ME/CFS169
Megaloblastic anemia170
Multiple Sclerosis171
Pancreatitis172
PCOS175
Poor endurance, weak grip (thiamine improved both in mice)176
Shingles177
Sleep Apnea178
Type 2 Diabetes179
Ulcerative colitis180
Food Sources of Thiamine:
Thiamine in foods is heat-sensitive and destroyed by prolonged boiling, high cooking temperatures, and degrades quicker when food is cooked at an alkaline pH (for example, baked with the addition of baking soda). Thiamine is also sensitive to UV light exposure.183
Thiamine in meat is retained better during braising than during deep frying or roasting. Since it is water soluble, boiling meats will leach thiamine into the cooking water. Freezing doesn’t destroy thiamine, so thiamine-rich foods that were previously frozen do not lose their thiamine.184185
The thiamine RDA is believed to be 1.2 mg, increasing to 1.4 mg in pregnancy and during lactation.
200 grams of sourdough bread, 160 grams of lean pork, 200 grams of pork heart and 250 ml of camel milk each meet the RDA. Together, half a litre of orange juice and one big mango meet half the RDA, as does about 1.5 cups (300 grams) of steamed brown rice.
Garlic
Oranges
Mangoes
Camel milk ⭐️
Sheep milk
Nutritional yeast⭐️
Pork (incl. raw cured ham, pork heart and pork liver) ⭐️
Hungarian red sweet pepper (it was recently discovered that it contains the same form of thiamine as garlic)186
Whole-grain long-fermented bread (either made with sourdough or yeast starter)
Long fermentation times increase the thiamine content of the dough, which is helpful, as during the baking process, up to 35% of the thiamine can be destroyed.187
“Thiamine concentrations were higher with long fermentation times in white bread (2.5 mg/g) compared to short fermentation (1.4 mg/g). Also, with longer fermentations, the thiamine content was significantly higher in white bread fermented with yeast.”188
My Preferred Vitamin B1 Supplements:
Adequate thiamine can be difficult to come by in foods, and it is one of the few vitamins that I believe nearly everyone would benefit from supplementing, at least in small amounts. This is partially because vitamin B1 can be depleted more rapidly than many other nutrients.
Source Naturals Coenzymated B1 Lozenges (Thiamine Pyrophosphate) ← my preferred supplement when first starting B1 therapy (bioactive, water soluble, less sulphur)
Metabolics Thiamine Pyrophosphate (used sublingually)
Swanson Benfotiamine ← fat-soluble, stronger
Objective Nutrients Thiamax (TTFD) ← most potent (fat-soluble, bypasses cellular transporters), best introduced later
Objective Nutrients ThiActive B (B Complex with TTFD & benfotiamine)
LifeBlud Energi+ (B Complex with benfotiamine)
How to Supplement Thiamine:
The remaining portions of this article, including a deep dive into vitamins B2 and B3, are available to paid subscribers only. If you aren’t a paid subscriber already, you can access the rest of this article by upgrading for $15 per month (cancel any time) or $100 for a yearly subscription.